Case Series/Study
(CS-166) Challenges in Cadaveric Skin Graft Survival in Transplant Recipients on Immunosuppressive Regimens
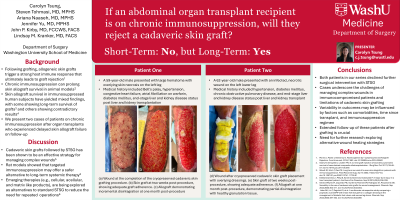
Methods: This article highlights two distinct cases, a 59-year-old and 62-year-old male with history of organ transplant requiring chronic immunosuppression who presented to our institution with injuries requiring skin graft placement. Cadaveric skin was used for grafting and although both grafts appeared to take up front, the grafts eventually failed.
Results:
A 59-year-old male with end-stage renal (ESRD) and liver disease (ESLD), chronic anemia, atrial fibrillation, hypertension, and liver/kidney transplantation 3 months prior presented with a large hematoma with overlying skin necrosis. Following debridement, a 25 x 9 cm cadaveric skin graft was applied to the lower left extremity wound with concurrent negative pressure wound therapy. Postoperatively, the patient’s immunosuppressive therapy was continued. The allograft demonstrated initial adherence but ultimately failed within 19 weeks. The patient was offered an elective STSG but preferred to continue with local wound care.
A 62-year-old male with a history of ESLD , ESRD secondary to diabetes/hypertension, and combined liver/kidney transplant 6 years prior presented with a left leg necrotizing soft tissue infection. After serial debridements, he received a 24 x 10 cm cadaveric skin graft and was continued on an appropriate immunosuppression regimen postoperatively. The graft initially adhered successfully but ultimately failed after 11 weeks. The patient was offered an elective STSG but declined in favor of local wound care.
Discussion: Our limited case series demonstrates how unreliable the use of cadaveric skin in transplant patients receiving immunosuppressive therapy can be over long-term follow-up. These cases underscore the need for extended follow-up, the development of new techniques to promote durable wound healing in immunosuppressed patients, and alternatives to traditional reoperative treatments, which many patients ultimately decline. Future research should focus on optimizing immunosuppressive protocols, exploring adjunctive therapies, and identifying predictive factors for allograft success to improve wound healing outcomes in this patient population.

.jpg)