Clinical Research
(CR-009) Clinical Efficacy of Ovine Forestomach Matrix and Collagen/oxidized Regenerated Cellulose for the Treatment of Venous Leg Ulcers: An Interim Analysis of Retrospective Comparative Real-world Evidence
Methods:
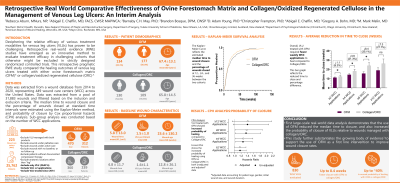
Cohorts consisted of VLUs treated with OFM or collagen/ORC. Data was extracted from a wound database from 2014 to 2020, representing 449 wound care centers across the United States. The median time to wound closure and the percentage of wounds closed at various timepoints were estimated using Kaplan-Meier survival analysis. The percentage of VLUs closed were statistically compared between treatment groups using Greenwood’s standard error estimates.
Results:
The 511 patients included in the study represented 830 total VLU, of which 470 were treated with OFM and 360 were treated with collagen/ORC. OFM demonstrated a significantly faster median time to closure (11.1±0.6 weeks) compared to the collagen/ORC group (12.3±1.0 weeks) (p=0.045). Cox proportional hazards analysis demonstrated that OFM-treated VLUs had significantly greater probability of healing (up to ~40%). The incidence of closure at 12-, 24- and 36-weeks was increased in OFM-treated VLUs relative to the collagen/ORC cohort.
Discussion: This interim analysis exemplifies the previously published PI surgical algorithm utilizing advanced biologic technology, such as OFM, as a reproducible, safe, and clinically effective treatment pathway to improve outcomes of challenging late-stage pressure injuries and potentially lower post-operative complication rates.

.jpg)