Clinical Research
(CR-043) Impact of a Nitric Oxide-generating Treatment in Diabetic Foot Ulcers Segmented by Infection Status and Wound Age: A Post-hoc Analysis
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Alan Horner, PhD – Head of Translational Sciences, Medical and Clinical Affairs, Convatec; Nicholas Boote, PhD – Director, Advanced Wound Care R&D, Convatec Ltd; Michael Edmonds, MD – Professor, Consultant Physician, Consultant Diabetologist, Diabetic Foot Clinic, King’s College Hospital, UK
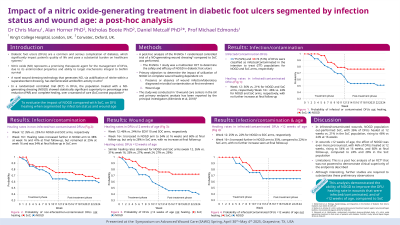
Introduction: Diabetic foot ulcers (DFUs) are a frequent and serious complication for patients with diabetes, which significantly impact patient quality of life and pose a substantial burden on healthcare systems. Nitric oxide (NO) represents a promising therapeutic agent for the management of DFUs, due to its antimicrobial properties and ability to target mechanisms integral to biofilm survival. The aim of this post-hoc analysis was to evaluate the effectiveness of a novel NO-generating wound dressing*, on the healing rates of infected DFUs segmented by infection status and wound age.
Methods: A post-hoc analysis of the ProNox1 randomised controlled trial1. The study involved treatment with either the NO-generating wound dressing* or Standard of Care (SoC), for 12 weeks or until the DFU had healed, and a further 12-week follow-up period. The impact of local infection status and wound age on the number of DFUs healed in the intention to treat (ITT) cohort were assessed.
Results: Of the 149 DFUs in the ITT cohort, 38/74 (51%) in the NO-generating dressing arm and 39/75 (52%) in the SoC arm were complicated by signs of infection at baseline. At week 12, healing rates in the infected DFUs were 36% vs 21% (NO-generating dressing arm vs SoC) and 35% vs 30% in those without infection. The healing trajectory continued in the NO-generating dressing arm, with 43.6% of DFUs healed by week 14, but no further improvement was seen in the SoC arm beyond week 12. In wounds ≤12 weeks in age, the healing rate in the treatment period was 52% for the NO-generating dressing arm and 22% for SoC. The healing rates increased in the follow-up period in both groups with 57% (NO-generating dressing arm) and 30% (SoC arm) of DFUs healed. In DFUs >12 weeks of age, the healing rates were the same for both arms: 25% in the study period and 30% at final follow-up. When segmented by the presence of local infection, the healing rate for the NO-generating dressing arm was 35% at final follow-up compared with 18% for SoC.
Discussion: This sub-analysis of the ProNox1 study data demonstrated the ability of the NO-generating wound dressing to improve the DFU healing rate in wounds of < 12 weeks of age and of infected wounds, compared with SoC.
Methods: A post-hoc analysis of the ProNox1 randomised controlled trial1. The study involved treatment with either the NO-generating wound dressing* or Standard of Care (SoC), for 12 weeks or until the DFU had healed, and a further 12-week follow-up period. The impact of local infection status and wound age on the number of DFUs healed in the intention to treat (ITT) cohort were assessed.
Results: Of the 149 DFUs in the ITT cohort, 38/74 (51%) in the NO-generating dressing arm and 39/75 (52%) in the SoC arm were complicated by signs of infection at baseline. At week 12, healing rates in the infected DFUs were 36% vs 21% (NO-generating dressing arm vs SoC) and 35% vs 30% in those without infection. The healing trajectory continued in the NO-generating dressing arm, with 43.6% of DFUs healed by week 14, but no further improvement was seen in the SoC arm beyond week 12. In wounds ≤12 weeks in age, the healing rate in the treatment period was 52% for the NO-generating dressing arm and 22% for SoC. The healing rates increased in the follow-up period in both groups with 57% (NO-generating dressing arm) and 30% (SoC arm) of DFUs healed. In DFUs >12 weeks of age, the healing rates were the same for both arms: 25% in the study period and 30% at final follow-up. When segmented by the presence of local infection, the healing rate for the NO-generating dressing arm was 35% at final follow-up compared with 18% for SoC.
Discussion: This sub-analysis of the ProNox1 study data demonstrated the ability of the NO-generating wound dressing to improve the DFU healing rate in wounds of < 12 weeks of age and of infected wounds, compared with SoC.

.jpg)