Clinical Research
(CR-045) Comparative Effectiveness of Skin Substitutes in Diabetic Foot and Venous Leg Ulcers from the Medicare Database
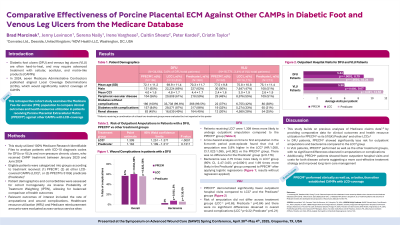
Diabetic foot ulcers (DFU) and venous leg ulcers (VLU) are often hard-to-heal, and may require advanced treatment with skin substitute products. In 2024, the seven Medicare Administrative Contractors published a Local Coverage Determination (LCD), which significantly restricts coverage of these products. This retrospective cohort study examines the Medicare Fee-for-service (FFS) population to compare clinical outcomes and health resources utilization in patients receiving Porcine Placental Extracellular Matrix (PPECM*) against other skin substitute products with LCD-coverage.
Methods:
This study analyzed 100% Medicare Research Identifiable Files (January 2020 - June 2024) for patients receiving a skin substitute treatment. Eligible patients were categorized into groups according to treatment received: (1) PPECM, (2) PPECM’s 510(k) predicate, (3) all other LCD-covered skin substitutes (LCSS). Patient demographics, comorbidities, and ulcer location were assessed for cohort homogeneity via inverse probability of treatment weighting (IPTW), allowing for balanced comparison of health outcomes.
Results:
A total of 34,664 patients with DFU (3.6% of DFU total patients) and 16,771 patients with VLU (3.4% of VLU total patients) received a skin substitute treatment. For the DFU cohort, patients receiving LCSS were 1.309 times more likely to undergo outpatient amputation than PPECM (95% CI 1.251 – 1.371, p< .0001), and bacteremia was 2.74 times more likely in LCSS (95% CI 2.471 – 3.053, p< .0001). In the VLU cohort, risk of amputation did not differ across treatment groups (p=.65). Across both wound types, PPECM demonstrated significantly fewer outpatient hospital visits compared to LCSS and the 510(k)-predicate (DFU: 5.84, 8.79, 10.24 respectively, p< .0001; VLU: 5.98, 9.07, 11.63, p< .0001). There were no differences in physician office visits, hospital admissions, and ER visits.
Discussion:
The findings suggest that PPECM performed clinically as well as or better than other covered skin substitutes. Notably, PPECM showed significantly less risk for outpatient amputations and wound complications in DFU patients. While PPECM patients had longer treatment durations and higher unique days of skin substitute applications, these patients showed fewer outpatient hospital visits and costs for both disease cohorts suggesting a more cost-effective treatment strategy and improved long-term care management.

.jpg)