Clinical Research
(CR-047) Impact of a Nitric Oxide-generating Wound Dressing in Diabetic Foot Ulcers in Patients Receiving Antibiotics: Post-hoc Analysis
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Chris Manu, MD FRCP – Consultant Diabetologist, Diabetic Foot Clinic, King’s College Hospital, UK; Alan Horner, PhD – Head of Translational Sciences, Medical and Clinical Affairs, Convatec; Michael Edmonds, MD – Professor, Consultant Physician, Consultant Diabetologist, Diabetic Foot Clinic, King’s College Hospital, UK
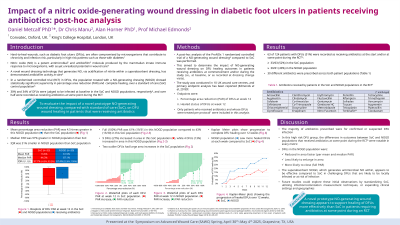
Introduction: Diabetic foot ulcers (DFUs) are a prevalent and serious complication of diabetes, which result in poor patient quality of life and substantial economic burden. Nitric oxide (NO) within a wound dressing represents a promising treatment for the management of DFUs, due to NO’s inherent antimicrobial properties. The purpose of this study was to evaluate the impact of a novel prototype NO-generating wound dressing*, compared with standard of care (SoC), on DFU wound healing in patients that were receiving antibiotics.
Methods: A post-hoc analysis of the ProNox 1 randomized controlled trial of a NO-generating wound dressing* compared to SoC was performed to determine the impact of NO-generating wound dressing* on DFU healing outcomes in patients receiving antibiotics at commencement and/or during the study. The study was conducted in 10 UK wound care centres, and primary endpoint analysis has been reported (Edmonds et al, 2018)1. The primary efficacy measure of this post-hoc analysis was DFU percent area reduction (PAR) at 12 weeks. A secondary efficacy measure was number of DFUs completely healed at 12 weeks.
Results: Of the 135 patients in the study, 71 (53%; 34 in SoC group; 37 in NO-generating wound dressing* group) were treated with 29 different antibiotics. At final assessment, the mean PAR was 48.7% in NO-generating wound dressing*-treated wounds, compared to 19.8% in the SoC group; a 59% greater PAR in NO-generating wound dressing* group. The number of healed (100% PAR) DFUs in the NO-generating wound dressing* was 14/37 (38%) and in the SoC group was 9/34 (26%).
Discussion: This sub-analysis demonstrates the ability of a NO-generating wound dressing* to improve DFU healing outcomes in patients that we being treated with antibiotics, compared with SoC.
Methods: A post-hoc analysis of the ProNox 1 randomized controlled trial of a NO-generating wound dressing* compared to SoC was performed to determine the impact of NO-generating wound dressing* on DFU healing outcomes in patients receiving antibiotics at commencement and/or during the study. The study was conducted in 10 UK wound care centres, and primary endpoint analysis has been reported (Edmonds et al, 2018)1. The primary efficacy measure of this post-hoc analysis was DFU percent area reduction (PAR) at 12 weeks. A secondary efficacy measure was number of DFUs completely healed at 12 weeks.
Results: Of the 135 patients in the study, 71 (53%; 34 in SoC group; 37 in NO-generating wound dressing* group) were treated with 29 different antibiotics. At final assessment, the mean PAR was 48.7% in NO-generating wound dressing*-treated wounds, compared to 19.8% in the SoC group; a 59% greater PAR in NO-generating wound dressing* group. The number of healed (100% PAR) DFUs in the NO-generating wound dressing* was 14/37 (38%) and in the SoC group was 9/34 (26%).
Discussion: This sub-analysis demonstrates the ability of a NO-generating wound dressing* to improve DFU healing outcomes in patients that we being treated with antibiotics, compared with SoC.

.jpg)