Case Series/Study
(CS-007) Hydromechanical Removal of Nonviable Tissue with Negative Pressure Wound Therapy and Instillation to Assist Limb Salvage
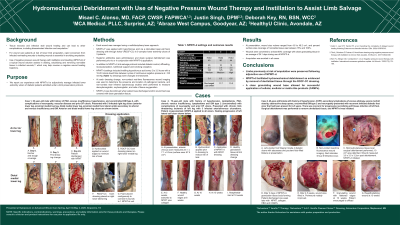
Tissue necrosis and infection stall wound healing and can lead to other complications, including disseminated infection and amputation.1 For wound care patients at risk of lower limb amputation, rapid conversion from infected nonhealing wounds to healing wounds is essential in avoiding amputation. Use of negative pressure wound therapy with instillation and dwelling (NPWTi-d) of a topical wound solution assists in diluting, solubilizing and removing nonviable tissue in infected wounds,2,3 which may help reverse a negative wound healing trajectory. We report our experience with NPWTi-d to adjunctively manage infected lower extremity ulcers of diabetic patients admitted under a limb salvage protocol.
Methods:
NPWTi-d was applied with hypochlorous acid via a reticulated open-cell foam dressing with through holes (ROCF-CC) in 9 complex lower extremity ulcers of 3 patients. Systemic antibiotics were administered, and sharp surgical debridement was performed prior to or in conjunction with NPWTi-d application. In addition to NPWTi-d, limb salvage protocol included diabetic control, offloading, revascularization, nutritional support and smoking cessation. NPWTi-d settings included instilling hypochlorous acid every 2 to 3.5 hours with a 10-20 minute dwell time between cycles of continuous negative pressure at -125 mmHg. At each dressing change, non-contact real-time fluorescence wound imaging was used to determine the presence and location of pathogenic bacteria, and non-contact near infrared spectroscopy studies were performed to measure deoxyhemoglobin, oxyhemoglobin, and ratio of tissue oxygenation (StO2). Dressings were changed 3 times/week. NPWTi-d was discontinued when patient was discharged and/or wound bed was covered with clean granulation tissue.
Results:
At presentation, wound size volume ranged from 4.6 to 49.2 cm3 and percent surface area coverage of nonviable tissue was between 15% and 100%. Wounds were converted to at least 90% coverage with clean granulating tissue in an average of 24.1 days during use of NPWTi-d. Amputation was avoided in all cases.
Discussion:
Limbs previously at risk of amputation were salvaged following adjunctive use of NPWTi-d. NPWTi-d facilitated hydromechanical debridement as evidenced by removal of devitalized tissue through the ROCF-CC dressing. A clean granulating wound base allowed for successful application of cellular, acellular or matrix-like products.

.jpg)
