Case Series/Study
(CS-141) Bacterial Species and Antimicrobial Resistance Patterns in Infected Wounds
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Introduction: Infection is one of the leading causes of delayed healing in chronic wounds. If left undiagnosed, wounds can remain stagnant for weeks, months, and even years. The goal of this retrospective study was to identify both the most prevalent high growth bacteria responsible for chronic wound infections as well as the antimicrobial resistance genes most commonly found within these bacteria. By identifying these, practitioners can implement targeted treatment plans to improve patient outcomes.
Methods: In this retroactive study, PCR wound cultures were collected from October 2023 to November 2024 from a suburban-based outpatient wound clinic. Out of all samples collected, 75 grew high loads of bacteria which were the only samples used in this study. Samples were obtained utilizing a “Z” pattern across the entire surface of the wound for ~ 15 seconds after sharp debridement and thorough cleansing of the wound bed.
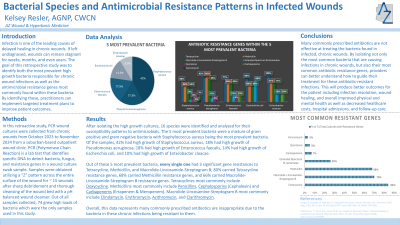
Results: After isolating the high growth cultures, 16 species were identified and then analyzed for their susceptibility patterns to antimicrobials. The 5 most prevalent bacteria were a mixture of gram positive and negative bacteria with Staphylococcus aureus being the most prevalent bacteria. Of the samples, 42% had high growth of Staphylococcus aureus, 18% had high growth of Pseudomonas aeruginosa, 18% had high growth of Enterococcus faecalis, 14% had high growth of Escherichia coli, and 10% had high growth of Enterobacter cloacae. Out of these 5 most prevalent bacteria, each had 3 significant gene resistances to Tetracycline, Methicillin, and Macrolide-Lincosamide-Streptogram B; 80% carried Tetracycline resistance genes, 68% carried Methicillin resistance genes, and 66% carried Macrolide-Lincosamide-Streptogram B resistance genes. Overall, this data represents that a large amount of commonly prescribed antibiotics may not be appropriate for wound infection treatment due to most often occurring bacterial infections being resistant.
Discussion: By isolating not only the most common bacteria that are causing infections in chronic wounds but also their antibiotic resistance genes, providers can better understand how to guide their treatment for these antibiotic-resistant infections. This will produce better patient outcomes for infection resolution, wound healing, and overall health as well as to decrease healthcare costs, hospital admissions, and follow-up care.
Methods: In this retroactive study, PCR wound cultures were collected from October 2023 to November 2024 from a suburban-based outpatient wound clinic. Out of all samples collected, 75 grew high loads of bacteria which were the only samples used in this study. Samples were obtained utilizing a “Z” pattern across the entire surface of the wound for ~ 15 seconds after sharp debridement and thorough cleansing of the wound bed.
Results: After isolating the high growth cultures, 16 species were identified and then analyzed for their susceptibility patterns to antimicrobials. The 5 most prevalent bacteria were a mixture of gram positive and negative bacteria with Staphylococcus aureus being the most prevalent bacteria. Of the samples, 42% had high growth of Staphylococcus aureus, 18% had high growth of Pseudomonas aeruginosa, 18% had high growth of Enterococcus faecalis, 14% had high growth of Escherichia coli, and 10% had high growth of Enterobacter cloacae. Out of these 5 most prevalent bacteria, each had 3 significant gene resistances to Tetracycline, Methicillin, and Macrolide-Lincosamide-Streptogram B; 80% carried Tetracycline resistance genes, 68% carried Methicillin resistance genes, and 66% carried Macrolide-Lincosamide-Streptogram B resistance genes. Overall, this data represents that a large amount of commonly prescribed antibiotics may not be appropriate for wound infection treatment due to most often occurring bacterial infections being resistant.
Discussion: By isolating not only the most common bacteria that are causing infections in chronic wounds but also their antibiotic resistance genes, providers can better understand how to guide their treatment for these antibiotic-resistant infections. This will produce better patient outcomes for infection resolution, wound healing, and overall health as well as to decrease healthcare costs, hospital admissions, and follow-up care.

.jpg)