Case Series/Study
(CS-173) A Multifunctional Dressing for Best Practices
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
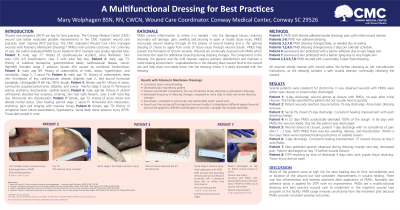
Introduction: Wound care programs (WCP) are key for best practices. The Conway Medical Center (CMC) wound care leader evaluated possible improvements in the CMC wound care practices. Goal: improve WCP practices. The CMC outpatient WCP managed wounds with Polymeric Membrane Dressings* (PMDs) with positive outcomes. For continuity of care, the author evaluated PMDs for an inpatient WCP. Example case studies reported here: Patient 1, Skin Tears (STs) left knee/forearm; Patient 2, right/left shoulder stage 2 pressure injuries (PIs); Patient 3, stage 2, 3 sacral PIs; Patient 4, unstageable PI left hip,100% slough; Patient 5 painful stage 2 sacral PI, Periwound skin swelling, erythema, discoloration. Patient 6, ST left forearm. Periwound skin discoloration; Patient 7, slow healing painful stage 2 sacral PI. Periwound skin maceration, erythema; Patient 8, sacral deep tissue pressure injury (DTPI).
Methods: Patient 1: PMD with silicone adhesive dressing; pain with initial wound cleanse. Patient’s 2-8: PMD non adhesive dressing. Patient 3,5,7,8: PMD dressing changed daily, as needed due to soiling. Patients 1,2,4,6 PMD dressing changed every 3 days per calendar schedule. All wounds initial cleanse with normal saline. No further cleansing as per manufacturer instructions.
Results: Several patients are inpatient for short time. It was observed wounds with PMDs were either near closure or closed when discharged. Patient 1: 4-day discharge, wound almost at closure with PMDs, no pain after initial cleanse. Patient 2: Patient wounds reached closure before 15-day discharge. Patient 3: Sacral PI closed before 25-day discharge. Patient 4: In 13 days PMDs autolytically debrided 80% slough. Patient 5: Wound almost at closure, patient 7-day discharge with no complaints of pain after 1 – 2 days. Patient 6: 3-day discharge, ST closed day 2. Patient 7: new epithelial growth after 1 dressing change, pain improved. Patient discharged before wound closure. Patient 8: DTPI resolving by time of discharge 3 days later, peri-wound skin healed.
Discussion: PMDs provided: consistent faster wound healing, decreased pain, cleaner wound bed, decreased frequency of dressing changes, atraumatic, ease of use. PMDs are a multifunctional dressing and best practice wound care to implement in the inpatient wound care program at this facility.
Methods: Patient 1: PMD with silicone adhesive dressing; pain with initial wound cleanse. Patient’s 2-8: PMD non adhesive dressing. Patient 3,5,7,8: PMD dressing changed daily, as needed due to soiling. Patients 1,2,4,6 PMD dressing changed every 3 days per calendar schedule. All wounds initial cleanse with normal saline. No further cleansing as per manufacturer instructions.
Results: Several patients are inpatient for short time. It was observed wounds with PMDs were either near closure or closed when discharged. Patient 1: 4-day discharge, wound almost at closure with PMDs, no pain after initial cleanse. Patient 2: Patient wounds reached closure before 15-day discharge. Patient 3: Sacral PI closed before 25-day discharge. Patient 4: In 13 days PMDs autolytically debrided 80% slough. Patient 5: Wound almost at closure, patient 7-day discharge with no complaints of pain after 1 – 2 days. Patient 6: 3-day discharge, ST closed day 2. Patient 7: new epithelial growth after 1 dressing change, pain improved. Patient discharged before wound closure. Patient 8: DTPI resolving by time of discharge 3 days later, peri-wound skin healed.
Discussion: PMDs provided: consistent faster wound healing, decreased pain, cleaner wound bed, decreased frequency of dressing changes, atraumatic, ease of use. PMDs are a multifunctional dressing and best practice wound care to implement in the inpatient wound care program at this facility.

.jpg)