Practice Innovations
(PI-011) Improved Outcomes in Surgical Reconstruction of Skin Defects: A Case Series Utilizing Fluorescence Imaging for Infection Management and Wound Bed Preparation
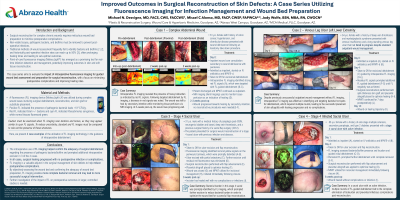
Surgical reconstruction for chronic wounds requires meticulous wound bed preparation to minimize postoperative complications. Non-viable tissues, bacteria, and biofilms must be removed to prevent post-operative infections. Traditional methods of wound assessment frequently fail to identify bacteria and biofilms1,2, and historically post-operative infection rates can reach up to 50%3, often leading to prolonged healing times. Point-of-care fluorescence imaging (MolecuLight®) has emerged as a promising tool for real-time infection detection and management, potentially improving outcomes in skin and soft tissue reconstruction. This technology detects and highlights bacterial presence above 104 CFU/gr in biofilm or planktonic form. This case series aims to evaluate the impact of intraoperative fluorescence imaging-guided wound bed assessment and preparation in surgical reconstruction with a focus on minimizing postoperative complications and improving healing rates.
Methods:
We present 5 challenging cases of chronic complex, wound candidates for that presented for surgical reconstruction. These included: Pressure ulcer on trunk n=2, VLU n=1, DFU n=1, Non-healing surgical wound on abdomen n=1. Intraoperative fluorescence imaging was performed in all 5 cases pre and post excisional debridement to monitor bacterial presence and location. The time to heal and incidence of postoperative complications, including post-operative infections, were measured.
Results: The intraoperative use of fluorescence imaging helped confirm the adequacy of surgical debridement regarding the presence of bacteria and prompted additional intraoperative excision in 3 of the 5 cases. In all 5 cases surgical healing progressed with no post operative infection. The pressure ulcer surgical reconstructions (n=2) healed without incident. The VLU, DFU, and non-healing surgical wound of the abdomen healed by secondary intention without further surgical intervention. Postoperative complications, particularly infection-related issues such as dehiscence, wound breakdown or surgical site infections, were 0%.
Discussion:
Intraoperative use of fluorescence imaging using MolecuLight is a valuable adjunct in the surgical management of skin defects to help reduce postoperative complications. By objectively assessing the wound bed and confirming the adequacy of wound bed preparation, fluorescence imaging enables more complete bacterial removal and may lead to more successful surgical intervention. Further investigation in larger, controlled studies is needed.

.jpg)