Practice Innovations
(PI-013) Evaluation of Negative Pressure Wound Therapy Using an All-in-one, Encapsulated, Reticulated Open-cell Foam Dressing in Complex Wounds
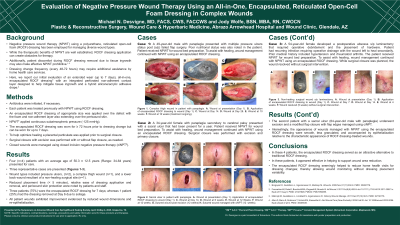
Negative pressure wound therapy (NPWT) using a polyurethane, reticulated open-cell foam (ROCF) dressing has been employed for managing diverse wound types. While NPWT’s therapeutic benefits are well established, ROCF dressing application can create obstacles for therapy. Additionally, patient discomfort during ROCF dressing removal due to tissue ingrowth may also make effective NPWT prohibitive.1-3 Dressing change frequency (every 48-72 hours) may require additional assistance by home health care services. Here, we report our evaluation of an extended wear (up to 7 days), all-in-one, encapsulated ROCF dressing* with an integrated perforated non-adherent contact layer designed to help mitigate tissue ingrowth and a hybrid silicone/acrylic adhesive drape.4
Methods: Antibiotics were initiated, if necessary. Each patient was treated previously with NPWT using ROCF dressing. An encapsulated ROCF dressing of appropriate size was applied over the defect with the foam and non-adherent layer also extending over the periwound skin. NPWT† applied continuous subatmospheric pressure (-125 mmHg). The encapsulated ROCF dressing was worn for ≥ 72 hours prior to dressing change but can be worn for up to 7 days.
Results:
Four (n=4) patients presented for care. Wound types included pressure ulcers, (n=2), a complex thigh wound (n=1), and a lower back wound resultant of a non-healing surgical site (n=1). Reduced placement time (< 5 minutes), relative ease of dressing application and removal, and periwound skin protection were noted by patients and staff. Three patients (75%) wore the encapsulated ROCF dressing for 7 days; whereas 1 patient (25%) experienced dressing removal at Day 6 due to soilage. Nevertheless, all patient wounds exhibited improvement evidenced by reduced wound dimensions and re-epithelialization. Interestingly, the appearance of wounds managed with NPWT using the encapsulated ROCF dressing were smooth, less granulated and accompanied by epithelialization relative to the characteristic appearance of ROCF dressing-treated wounds.
Discussion:
In these 4 patients, the encapsulated ROCF dressing served as an attractive alternative to traditional ROCF dressing. In these patients, it appeared effective in helping to support wound area reduction. The encapsulated ROCF dressing seemingly helped to reduce home health visits for dressing changes; thereby allowing wound monitoring without dressing placement variability.

.jpg)
