Practice Innovations
(PI-015) Impact of Implementing a Soft Silicone Multi-layered Foam Dressing Protocol for Pressure Injury Prevention on Incidence and Severity
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Mandy Spitzer, MBA, RN, CWOCN, CFCN
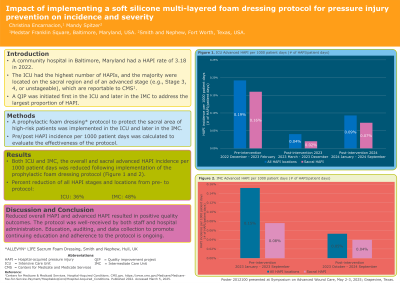
Introduction: A community hospital in Baltimore, Maryland had a hospital-acquired pressure injury (HAPI) rate of 3.18 in 2022, with the intensive care unit (ICU) having the highest number of HAPIs. The majority of these HAPIs were found on the sacral region, of which many were on the sacrum and of an advanced stage (e.g., Stage 3, 4, or unstageable). Due to the high human1,2 and economic3,4 burden of HAPI, the inpatient WOC nurses, quality department, and ICU leaders convened in , January 2023 to discuss ways to improve the ICU HAPI rate as well as the overall severity. The team agreed that in addition to the current standard preventative measures, an additional method was needed to address sacral HAPIs.
Methods: A protocol was developed for the application of a prophylactic foam dressing to the sacral area for all qualifying patients. In February 2023, the ICU received education and began implementation of the new protocol. A clinical nurse completed chart audits to track adherence to the new protocol and provided real-time, peer-to-peer feedback to the ICU nursing staff. Prophylactic dressing usage was also reinforced during WOC nurse rounding. As a result of the outcomes, the protocol was later expanded to Intermediate Care (IMC) in September 2023.
Results: Pre-intervention HAPI incidence was collected and analyzed. Post-intervention data was collected in the ICU from March to September 2024 and in the IMC from September 2023 to September 2024. In the 3 months prior to implementation of the dressing, there were 6 incidences of advanced HAPIs in the ICU. In the 7 months following implementation of the protocol there were no reported advanced HAPI. Following implementation of the protocol a downward trend in HAPI rates has been recorded with data collection ongoing.
Discussion: Reduced overall HAPI and severity resulted in positive patient, clinical, and economic outcomes. As a result, the protocol was well-received by both staff and hospital administration. Continued education, auditing, and data collection to promote continuing education and adherence to the protocol is ongoing.
Methods: A protocol was developed for the application of a prophylactic foam dressing to the sacral area for all qualifying patients. In February 2023, the ICU received education and began implementation of the new protocol. A clinical nurse completed chart audits to track adherence to the new protocol and provided real-time, peer-to-peer feedback to the ICU nursing staff. Prophylactic dressing usage was also reinforced during WOC nurse rounding. As a result of the outcomes, the protocol was later expanded to Intermediate Care (IMC) in September 2023.
Results: Pre-intervention HAPI incidence was collected and analyzed. Post-intervention data was collected in the ICU from March to September 2024 and in the IMC from September 2023 to September 2024. In the 3 months prior to implementation of the dressing, there were 6 incidences of advanced HAPIs in the ICU. In the 7 months following implementation of the protocol there were no reported advanced HAPI. Following implementation of the protocol a downward trend in HAPI rates has been recorded with data collection ongoing.
Discussion: Reduced overall HAPI and severity resulted in positive patient, clinical, and economic outcomes. As a result, the protocol was well-received by both staff and hospital administration. Continued education, auditing, and data collection to promote continuing education and adherence to the protocol is ongoing.

.jpg)