Evidence-Based Practice
(EBP-006) Impacts of Medicare/medicaid Status on Venous Leg Ulcer Outcomes
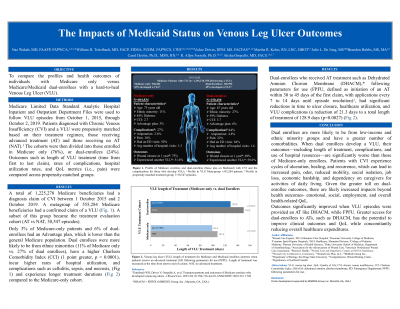
The socioeconomic status of dual-enrolees includes near poverty status, a significant increase in ethnic minorities, and high rates of comorbidities compared to their Medicare-only counterparts. His study quantified race, gender, comorbidities, Medicaid status, and health outcomes for those who develop hard-to-heal venous leg ulcers (VLU) from two groups; those covered by Medicare-only versus those with Medicare and Medicaid (dual-enrolees).
Methods:
Medicare Limited Data Standard Analytic Hospital Inpatient and Outpatient Department Files were used to follow episodes of medical care for a VLU from October 1, 2015, through October 2, 2019. Propensity matched groups were split into patients enrolled in Medicare-only (73%) and those enrolled in Medicare and Medicaid (dual-enrolees, 27%). Episode claims were used to document demographics, comorbidities, outcomes and Quality of Life (QoL) metrics.
Results:
Twenty-seven percent of the 555,284 Medicare beneficiaries evaluated in this analysis were Medicare/Medicaid dual-enrolees. To qualify for Medicaid, their income had to be below 133% of the federal poverty level. Only 3% of Medicare-only patients and 6% of dual-enrolees had an Advantage plan, lower than the general Medicare population. Dual-enrolees, compared to those covered by Medicare-only demonstrated a Charlson Comorbidity Index (CCI) score 1 point greater (p < 0.0001), a 16% increase in ethnic minorities, lengths of treatment that were 16 days longer with significantly higher rates of infection, hospital utilization, and costs. Dual-enrolees who received early and regularly applied cellular acellular, matrix-like products (CAMPs), such as DHACM, saw significant reductions in time to ulcer closure, healthcare utilization, and VLU complications.
Discussion:
Dual-enrolee VLUs take longer to close, develop more complications, and use significantly more hospital resources and expenses. Outcomes significantly improved when VLU episodes were provided DHACM, while following parameters for use (FPFU). Greater access to CAMPs has the potential to improve clinical outcomes and QoL while concomitantly reducing overall healthcare expenditures.

.jpg)