Health Economics
(HE-008) Cost-analysis of Universal Decolonization with Pure Hypochlorous Acid and Mupirocin to Prevent Infections in Burn Patients
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Debashish Chakravarthy, PhD; Kevin Foster, MD
Introduction:
Burn patients are particularly susceptible to infections, including Methicillin-resistant Staphylococcus aureus (MRSA). MRSA can originate from their own flora or the environment, and it is a leading cause of morbidity and mortality. Universal decolonization has been shown to reduce infection rates. The objective of this study was to conduct a cost-analysis of pure hypochlorous acid (pHA) and mupirocin for the prevention of MRSA infection in hospitalized burn patients.
Methods:
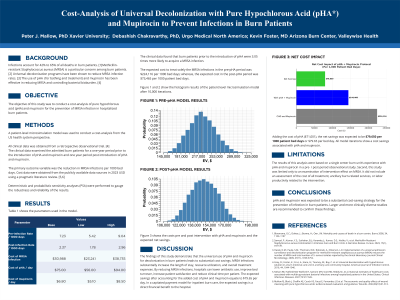
A patient-level microsimulation model was used to conduct a cost-analysis from the US health system perspective. All clinical data was obtained from a retrospective observational trial. [1] The clinical data examined the admitted burn patients for a one-year period prior to the introduction of pHA and mupirocin and one year period post introduction of pHA and mupirocin. The primary outcome variable was the reduction in MRSA infections per 1000 bed days. Cost data were obtained from the publicly available data sources in 2023 USD using a pragmatic literature review. [2,3] Deterministic and probabilistic sensitivity analyses (PSA) were performed to gauge the robustness and reliability of the results.
Results:
The clinical data found that burn patients prior to the introduction of pHA were 3.05 times more likely to acquire a MRSA infection. The expected cost to treat solely the MRSA infections in the pre-pHA period was $224,116 per 1000 bed days; whereas, the expected cost in the post-pHA period was $73,465 per 1000 patient bed days. Adding the cost of pHA, the net savings was expected to be $79,650 per 1000 patient bed days or $79.65 per bed day. The sensitivity analyses revealed that these results were robust and reliable to changes in the parameter values.
Discussion:
pHA and mupirocin was expected to be a substantial cost-saving strategy for the prevention of infection in burn patients. Larger and more clinically diverse studies are recommended to confirm these findings.
Burn patients are particularly susceptible to infections, including Methicillin-resistant Staphylococcus aureus (MRSA). MRSA can originate from their own flora or the environment, and it is a leading cause of morbidity and mortality. Universal decolonization has been shown to reduce infection rates. The objective of this study was to conduct a cost-analysis of pure hypochlorous acid (pHA) and mupirocin for the prevention of MRSA infection in hospitalized burn patients.
Methods:
A patient-level microsimulation model was used to conduct a cost-analysis from the US health system perspective. All clinical data was obtained from a retrospective observational trial. [1] The clinical data examined the admitted burn patients for a one-year period prior to the introduction of pHA and mupirocin and one year period post introduction of pHA and mupirocin. The primary outcome variable was the reduction in MRSA infections per 1000 bed days. Cost data were obtained from the publicly available data sources in 2023 USD using a pragmatic literature review. [2,3] Deterministic and probabilistic sensitivity analyses (PSA) were performed to gauge the robustness and reliability of the results.
Results:
The clinical data found that burn patients prior to the introduction of pHA were 3.05 times more likely to acquire a MRSA infection. The expected cost to treat solely the MRSA infections in the pre-pHA period was $224,116 per 1000 bed days; whereas, the expected cost in the post-pHA period was $73,465 per 1000 patient bed days. Adding the cost of pHA, the net savings was expected to be $79,650 per 1000 patient bed days or $79.65 per bed day. The sensitivity analyses revealed that these results were robust and reliable to changes in the parameter values.
Discussion:
pHA and mupirocin was expected to be a substantial cost-saving strategy for the prevention of infection in burn patients. Larger and more clinically diverse studies are recommended to confirm these findings.

.jpg)