Health Economics
(HE-012) Disproving Misconceptions Surrounding Workflow Efficiency in a Hospital-based Wound Center with the Autologous Multilayered Leukocyte, Platelet, and Fibrin Patch
< A novel treatment for diabetic foot ulcers (DFUs) is the autologous multilayered leukocyte, platelet, and fibrin patch (MLPF Patch). While a randomized controlled trial1 was conducted to prove its efficacy, providers and program directors may be concerned that the time for this procedure would negatively impact the workflow of the wound center. When reviewing our efficiency, we were curious to determine if the use of the MLPF Patch did alter our workflow and how the time differed from other treatments.
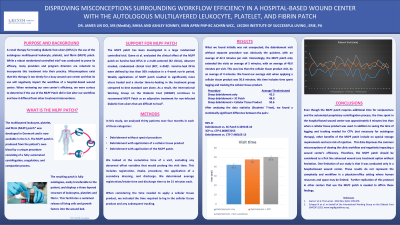
Methods: In this study, we analyzed 30 consecutive patients over 4 months in these categories: Debridement without special procedure, debridement with application of a cellular tissue product, and debridement with application of the MLPF patch. We looked at the accumulative time of a visit, excluding any abnormal variables that would prolong the visit time. Time measured included registration, intake, procedure, the application of a secondary dressing, and discharge.
Results: Our initial findings were as expected; the debridement visit without separate procedure was the quickest, with an average of 42.3 minutes per visit. Interestingly, the MLPF patch only extended the visits an average of ~6 minutes. This was less than the cellular tissue product visit, which was an average of 50.6 minutes, including time spent logging and tracking the product. The misconception that the MLPF patch would take longer did not prove true. Due to the positive outcomes, the automated process, and no logging or tracking requirements, we are more inclined to use the MLPF patch.
Discussion: Even though the MLPF patch requires additional time for venipuncture and the centrifugation process, the time spent in the hospital-based wound center was approximately 4 minutes less than when a cellular tissue product was used. In addition to saving time of logging and tracking needed for CTPs, other benefits of the MLPF patch include no special storage requirements and zero risk of rejection. This data disproves the common misconceptions of slowing workflow and negatively impacting a wound center’s efficiency. Therefore, the MLPF patch should be considered as a first line advanced wound care treatment without hesitation. One limitation of our study is that it was conducted in a hospital-based wound center. These results do not represent the complexity and workflow in a physician-office setting where human resources and space may be limited. Also, further replication of this protocol in other centers that use the MLPF patch is needed to affirm these findings.

.jpg)