Case Series/Study
(CS-160) Concurrent Use of a GV/MB PVA Wide-cell Antibacterial Foam with Negative Pressure Wound Therapy
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
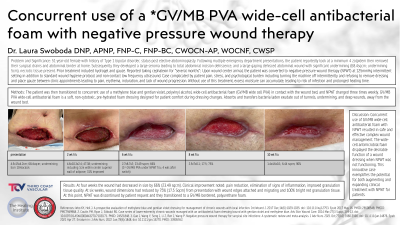
Introduction: Problem: 51-year-old female with history of Type 1 bipolar disorder, status-post elective abdominoplasty. Following multiple emergency department presentations, the patient reportedly took at a minimum 4 zolpidem then removed their surgical drains and abdominal binder at home. Subsequently they developed a large seroma leading to total abdominal incision dehiscence, and a large gaping dehisced abdominal wound with significant undermining (68.4sqcm; undermining 5cm), necrotic tissue present.
Significance: Prior treatment included hydrogel and gauze. Upon wound center arrival, the patient was converted to negative pressure wound therapy (NPWT) at 125mmHg intermittent setting in addition to standard wound hygiene protocol and non-contact low frequency ultrasound. Case complicated by patient pain, stress, and psychological burden including turning the machine off intermittently and refusing to remove dressing and place gauze between clinic appointments leading to pain, erythema, induration, and lack of wound progression.
Methods: The patient was then transitioned to concurrent use of a methylene blue and gentian violet, polyvinyl alcohol, wide-cell, antibacterial foam (GV/MB wide cell PVA) in contact with the wound bed, and NPWT changed three times weekly.
Results: At four weeks the wound had decreased in size by 66% (23.49 sqcm). Clinical improvement noted: pain reduction, elimination of signs of inflammation, improved granulation tissue quality. At six weeks, wound dimensions had reduced by 75% (17.5 Sqcm) from presentation with wound edges attached and migrating and 100% bright red granulation tissue. At this point, NPWT was discontinued by patient request and they transitioned to a GV/MB bordered, poly urethane foam.
Discussion: Concurrent use of GV/MB wide cell PVA with NPWT resulted in safe and effective complex wound management. The wide-cell antimicrobial foam displayed the desirable function of a wound dressing when NPWT was not functioning. This innovative case exemplifies the potential for both augmenting and expanding clinical treatment with NPWT for patients.
Significance: Prior treatment included hydrogel and gauze. Upon wound center arrival, the patient was converted to negative pressure wound therapy (NPWT) at 125mmHg intermittent setting in addition to standard wound hygiene protocol and non-contact low frequency ultrasound. Case complicated by patient pain, stress, and psychological burden including turning the machine off intermittently and refusing to remove dressing and place gauze between clinic appointments leading to pain, erythema, induration, and lack of wound progression.
Methods: The patient was then transitioned to concurrent use of a methylene blue and gentian violet, polyvinyl alcohol, wide-cell, antibacterial foam (GV/MB wide cell PVA) in contact with the wound bed, and NPWT changed three times weekly.
Results: At four weeks the wound had decreased in size by 66% (23.49 sqcm). Clinical improvement noted: pain reduction, elimination of signs of inflammation, improved granulation tissue quality. At six weeks, wound dimensions had reduced by 75% (17.5 Sqcm) from presentation with wound edges attached and migrating and 100% bright red granulation tissue. At this point, NPWT was discontinued by patient request and they transitioned to a GV/MB bordered, poly urethane foam.
Discussion: Concurrent use of GV/MB wide cell PVA with NPWT resulted in safe and effective complex wound management. The wide-cell antimicrobial foam displayed the desirable function of a wound dressing when NPWT was not functioning. This innovative case exemplifies the potential for both augmenting and expanding clinical treatment with NPWT for patients.

.jpg)