Case Series/Study
(CS-063) Hidradenitis Suppurativa Revision Surgery with Split-thickness Skin Graft After Contracture Development Following Primary Closure: A Case Report
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Julia McGee, BS – Medical Student, Tulane University School of Medicine; Laurel Adams, BS; Leely Rezvani, MD – Resident, General Surgery, Tulane University School of Medicine; Abigail Chaffin, MD, FACS, CWSP, MAPWCA – Professor, Plastic Surgery, Tulane University School of Medicine
Introduction: Hidradenitis suppurativa (HS) is a chronic and debilitating inflammatory skin condition necessitating a multidisciplinary approach, including medical management, surgical intervention, and wound care. The disease is associated with lifestyle factors like smoking and obesity and has known genetic predispositions; however, its pathophysiology remains incompletely understood (4). HS frequently involves areas such as the axilla, inner thighs, and genitalia, causing significant physical discomfort and profound psychosocial impacts due to visible, painful lesions (3). Patients often pursue extensive treatments to mitigate the disabling effects of HS. While surgical excision is a cornerstone of therapy, complications such as infection, dehiscence, and scar contractures are common (2).
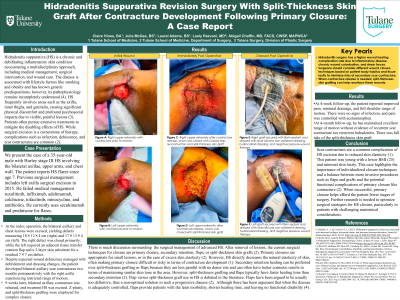
Methods: We present the case of a 35-year-old male with Hurley stage III HS involving the bilateral axillae, upper arms, and chest wall. On 8/29, the bilateral axillary and chest lesions were excised, yielding defects measuring 18×12×4 cm (right) and 17×13×4 cm (left). The right defect was closed primarily, while the left required an adjacent tissue transfer rotation flap and a 3-layer skin substitute for a residual 7×7 cm defect.
Despite expected wound dehiscence managed with debridement and dressing changes, the patient developed right axillary scar contractures two months postoperatively with the right axilla experiencing restricted range of motion.
On 11/7, right axillary contracture was released, and recurrent HS was excised. Z-plasty,, and split-thickness grafting were employed for complex closure.
Results: At follow-up on 12/11, the patient reported improved pain, minimal drainage, and full shoulder range of motion. There were no signs of infection, and pain was controlled with acetaminophen.
Discussion: Scar contractures are a common complication of HS excision due to reduced skin elasticity (1). This patient was young with a lower BMI (25) and minimal skin laxity. This case highlights the importance of individualized closure techniques and a balance between more invasive procedures such as flaps and grafts and the potential functional complications of primary closure like contracture (2). When successful, primary closure helps afford the patient fewer stages of surgery. Further research is needed to optimize surgical strategies for HS closure, particularly in patients with challenging anatomical considerations.
Methods: We present the case of a 35-year-old male with Hurley stage III HS involving the bilateral axillae, upper arms, and chest wall. On 8/29, the bilateral axillary and chest lesions were excised, yielding defects measuring 18×12×4 cm (right) and 17×13×4 cm (left). The right defect was closed primarily, while the left required an adjacent tissue transfer rotation flap and a 3-layer skin substitute for a residual 7×7 cm defect.
Despite expected wound dehiscence managed with debridement and dressing changes, the patient developed right axillary scar contractures two months postoperatively with the right axilla experiencing restricted range of motion.
On 11/7, right axillary contracture was released, and recurrent HS was excised. Z-plasty,, and split-thickness grafting were employed for complex closure.
Results: At follow-up on 12/11, the patient reported improved pain, minimal drainage, and full shoulder range of motion. There were no signs of infection, and pain was controlled with acetaminophen.
Discussion: Scar contractures are a common complication of HS excision due to reduced skin elasticity (1). This patient was young with a lower BMI (25) and minimal skin laxity. This case highlights the importance of individualized closure techniques and a balance between more invasive procedures such as flaps and grafts and the potential functional complications of primary closure like contracture (2). When successful, primary closure helps afford the patient fewer stages of surgery. Further research is needed to optimize surgical strategies for HS closure, particularly in patients with challenging anatomical considerations.

.jpg)