Clinical Research
(CR-076) Affects of Long Limb Discrepancy on Temporospatial Gait Parameters and the Development of Diabetic Ulcers Using Computer Assisted Gait Analysis
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Ronald Sherman, DPM MBA; Caitlin Hicks, MD; Jay Segel, DPM; Mark Hopkins, PT CPO MBA; Brian Murray, PT; Sally Crawford, MS; Tracy Winchester, N/A
Introduction: Diabetes mellitus is the most rapidly growing cause of the global disease burden. DFUs are a manifestation of diabetes associated with difficult/delayed wound healing and a five-year mortality rate of 13-42%. Prevention and effective management of DFUs is crucial to reduce the risk of lower limb amputations and improve the quality of life for patients with diabetes. Currently, there is greater focus on treatment of existing DFUs rather than prevention, despite a majority of these conditions being entirely preventable. The current standard of care in ulcer prevention is a custom-molded or depth-inlay shoe mandated by US Congress in 1987 despite lack of convincing evidence on their clinical effectiveness. Computer assisted gait analysis (CAGA) is an emerging technology that allows physicians to see the unseen. Comprehension of abnormal diabetic gait increases the effectiveness of diabetic shoes and orthotics through customized correction of temporospatial gait parameters. We seek to measure the affects of long leg limb discrepancy on the development of abnormal gait leading to diabetic ulceration through the use of CAGA.
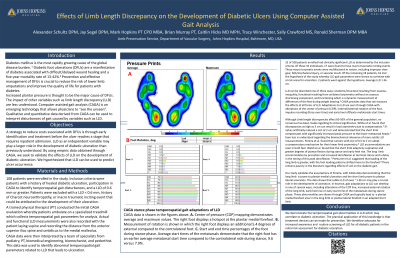
Methods: 100 patients with a history of healed diabetic ulcer underwent CAGA testing to identify locations of peak plantar pressure during gait cycle. Physical assessment of limb lengths was conducted to identify patients with long leg discrepancy. Patients with limb length discrepancy were compared to a control group of patients without long limbs to identify altered gait parameters leading to diabetic ulceration.
Results: Patients with limb length discrepancies were found to have altered gait parameters leading to increased propensity to develop diabetic ulceration and amputation. We are able to quantify and qualify these gait metrics in order to predict where ulceration is likely to occur in patients with a long limb. We demonstrate a positive correlation of long leg discrepancy with increased peak plantar pressure measurements comparative to the contralateral limb.
Discussion: These data are able to be used clinically to create orthotic solutions targeted to address long limb discrepancy. We are able to address predicable gait trends that are caused by limb length discrepancy to prevent reulceration and amputation.
Methods: 100 patients with a history of healed diabetic ulcer underwent CAGA testing to identify locations of peak plantar pressure during gait cycle. Physical assessment of limb lengths was conducted to identify patients with long leg discrepancy. Patients with limb length discrepancy were compared to a control group of patients without long limbs to identify altered gait parameters leading to diabetic ulceration.
Results: Patients with limb length discrepancies were found to have altered gait parameters leading to increased propensity to develop diabetic ulceration and amputation. We are able to quantify and qualify these gait metrics in order to predict where ulceration is likely to occur in patients with a long limb. We demonstrate a positive correlation of long leg discrepancy with increased peak plantar pressure measurements comparative to the contralateral limb.
Discussion: These data are able to be used clinically to create orthotic solutions targeted to address long limb discrepancy. We are able to address predicable gait trends that are caused by limb length discrepancy to prevent reulceration and amputation.

.jpg)