Clinical Research
(CR-023) Clinically Validated Non-invasive Automated Burn Diagnostic System for Healthcare Using artificial Intelligence: AMBUSH-AI
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Md Masudur Rahman, PhD – Post-Doctoral, Computer Science, Purdue University, West Lafayette, IN 47907; Surya Gnyawali, PhD – Research assistant professor, Surgery, University of Pittsburgh, Pittsburgh, PA,15219; Yexiang Xue, PhD – Assistant Professor, Computer Science, Purdue University, West Lafayette, IN 47907; Juan Wachs, PhD – Professor, School of Industrial Engineering, Purdue University, West Lafayette, IN 47907; Gayle Gordillo, PhD – Professor, Plastic Surgery, University of Pittsburgh, Pittsburgh, PA,15219
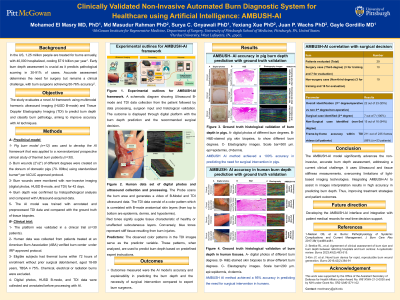
Introduction: In the US, 1.25 million people are treated for burns annually, with 40,000 hospitalized, costing $7.9 billion per year. Early burn depth assessment is crucial as it predicts pathological scarring in 30-91% of cases. Accurate assessment determines the need for surgery but remains a clinical challenge, with burn surgeons achieving 50-76% accuracy. The study evaluates a novel AI framework using multimodal harmonic ultrasound imaging (HUSD B-mode) and Tissue Doppler Elastography Imaging (TDI) to predict burn depth and classify burn pathology, aiming to improve accuracy with AI techniques.
Methods: A pig burn model (n=12) was used to develop the AI framework that was applied to a nonrandomized prospective clinical study of thermal burn patients (n=30). Burn wounds (2”x2”) of different degrees were created on the dorsum of domestic pigs (70-80lbs) using standardized burner. Burn wounds were monitored with non-invasive imaging (digital photos, HUSD B-mode, and TDI) for 42 days. Burn depth was confirmed by histopathological analysis and compared with Ultrasound-acquired data. The AI model was trained with annotated and preprocessed TDI data. The platform was validated in a clinical trial (n=30 patients), eligible subjects had thermal burns within 72 hours of enrollment without prior surgical debridement, aged 18-89 years, TBSA ≤ 75%. Chemical, electrical or radiation burns were excluded. Outcomes measured were the AI model’s accuracy and explainability in predicting the burn depth and the necessity of surgical intervention compared to expert burn surgeons.
Results: HUSD B-mode and TDI identified unique biomechanical and biological burn response patterns, validated by H&E and Trichrome staining in human and pigs. The observed color patterns in the TDI images served as the predictor variable. These patterns, when analyzed, are used to predict burn depth based on predefined expert instructions. Thirty patients (47.6± 17.6 years old, BMI= 28.8 ± 5.3 kg/m², TBSA = 7.7 ± 8.5 %) were enrolled. The AMBUSH-AI achieved 95% accuracy in predicting the need for surgical intervention in humans and 100% accuracy of third-degree burns prediction in pigs, with 100% sensitivity and F1-score of 93%. The pig model demonstrated the algorithm's precision and reliability. Validation with human data confirmed its clinical accuracy.
Discussion: The AMBUSH-AI model significantly advances the non-invasive, accurate burn depth assessment, addressing a current clinical challenge. It uses Ultrasound and tissue stiffness measurements, overcoming limitations of light-based imaging technologies. Integrating AMBUSH-AI to assist in images interpretation results in high accuracy in predicting burn depth. Thus, improving treatment strategies and patient outcomes.
Methods: A pig burn model (n=12) was used to develop the AI framework that was applied to a nonrandomized prospective clinical study of thermal burn patients (n=30). Burn wounds (2”x2”) of different degrees were created on the dorsum of domestic pigs (70-80lbs) using standardized burner. Burn wounds were monitored with non-invasive imaging (digital photos, HUSD B-mode, and TDI) for 42 days. Burn depth was confirmed by histopathological analysis and compared with Ultrasound-acquired data. The AI model was trained with annotated and preprocessed TDI data. The platform was validated in a clinical trial (n=30 patients), eligible subjects had thermal burns within 72 hours of enrollment without prior surgical debridement, aged 18-89 years, TBSA ≤ 75%. Chemical, electrical or radiation burns were excluded. Outcomes measured were the AI model’s accuracy and explainability in predicting the burn depth and the necessity of surgical intervention compared to expert burn surgeons.
Results: HUSD B-mode and TDI identified unique biomechanical and biological burn response patterns, validated by H&E and Trichrome staining in human and pigs. The observed color patterns in the TDI images served as the predictor variable. These patterns, when analyzed, are used to predict burn depth based on predefined expert instructions. Thirty patients (47.6± 17.6 years old, BMI= 28.8 ± 5.3 kg/m², TBSA = 7.7 ± 8.5 %) were enrolled. The AMBUSH-AI achieved 95% accuracy in predicting the need for surgical intervention in humans and 100% accuracy of third-degree burns prediction in pigs, with 100% sensitivity and F1-score of 93%. The pig model demonstrated the algorithm's precision and reliability. Validation with human data confirmed its clinical accuracy.
Discussion: The AMBUSH-AI model significantly advances the non-invasive, accurate burn depth assessment, addressing a current clinical challenge. It uses Ultrasound and tissue stiffness measurements, overcoming limitations of light-based imaging technologies. Integrating AMBUSH-AI to assist in images interpretation results in high accuracy in predicting burn depth. Thus, improving treatment strategies and patient outcomes.

.jpg)