Clinical Research
(CR-029) Impact of Digital Wound Care: A Pilot Study at Giishkaandago’ikwe Health Services
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Heba Tallah Mohammed, PhD – Swift Medical Inc.; Deirdre Drombolis, BSN, RN, WCC; Kaitlyn Ramsay, PhD – University of Toronto; Samiha Mohsen, MSc – University of Toronto; Samantha Bestavros, MSc – University of Toronto; Sheila Wang, MD,PhD – Women College Hospital; Robert D. J. Fraser, MN RN NSWOC WOCC(C) – Swift Medical Inc.
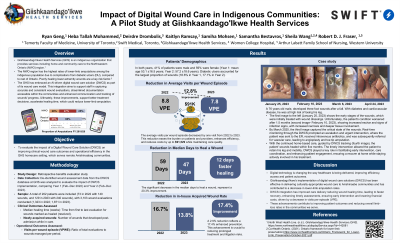
Introduction: Chronic wounds impose high physical, psychosocial burden on patients and costs on healthcare systems. 1 Artificial intelligence (AI)-based systems have been developed with capabilities including measuring wound dimensions to provide objective wound tracking and support wound care decision-making.2 However, their real-world impact on clinical outcomes and operational efficiency remains unexplored. 3 This study aims to evaluate the impact of an AI-driven digital wound care solution (DWCS) on clinical and operational outcomes for the indigenous First Nation community served by Giishkaandago’Ikwe Health Services.
Methods: This retrospective benefits evaluation study analyzed clinical and operational outcomes of the DWCS in Giishkaandago’Ikwe Health Services from February 2022 to December 2023. Leveraging the comprehensive and clinically validated DWCS database, the study compared performance metrics immediately following the implementation of a digital wound care solution (Year 1, February – December 2022) to outcomes one year later (Year 2, February – December 2023). Clinical outcome metrics included median days to heal and number of newly acquired wounds during management. Operational outcome metrics included visits per wound, evaluations completed within 24 hours and nursing staff optimization.
Results: A total of 202 patients (59% male, 41% female) comprising 380 wounds and 3,194 wound evaluations were analyzed. The most common wound types included pressure injuries (18.9%, 72/380), surgical wounds (18.7%, 71/380) and diabetic ulcers (17.6%, 67/380). Clinical outcomes included a 20% reduction in median days to heal and a 2.9% reduction in newly acquired wounds while under management. Operationally, there was a 12.8% reduction in the number of visits per wound, translating into ~$91,529 in cost savings. There was also a 9.7% increase in the proportion of wound evaluations documented, reviewed and completed within 24 hours. Additionally, there was a 9% increase in the utilization of registered practical nurses (RPNs) for wound assessments, allowing registered nurses (RNs) to dedicate more time to high-risk patients.
Discussion: The AI-based digital wound care system substantially improved clinical and operational outcomes for Giishkaandago’Ikwe Health Services and the communities it serves, potentially by improving wound tracking, monitoring and workflow efficiency.
Methods: This retrospective benefits evaluation study analyzed clinical and operational outcomes of the DWCS in Giishkaandago’Ikwe Health Services from February 2022 to December 2023. Leveraging the comprehensive and clinically validated DWCS database, the study compared performance metrics immediately following the implementation of a digital wound care solution (Year 1, February – December 2022) to outcomes one year later (Year 2, February – December 2023). Clinical outcome metrics included median days to heal and number of newly acquired wounds during management. Operational outcome metrics included visits per wound, evaluations completed within 24 hours and nursing staff optimization.
Results: A total of 202 patients (59% male, 41% female) comprising 380 wounds and 3,194 wound evaluations were analyzed. The most common wound types included pressure injuries (18.9%, 72/380), surgical wounds (18.7%, 71/380) and diabetic ulcers (17.6%, 67/380). Clinical outcomes included a 20% reduction in median days to heal and a 2.9% reduction in newly acquired wounds while under management. Operationally, there was a 12.8% reduction in the number of visits per wound, translating into ~$91,529 in cost savings. There was also a 9.7% increase in the proportion of wound evaluations documented, reviewed and completed within 24 hours. Additionally, there was a 9% increase in the utilization of registered practical nurses (RPNs) for wound assessments, allowing registered nurses (RNs) to dedicate more time to high-risk patients.
Discussion: The AI-based digital wound care system substantially improved clinical and operational outcomes for Giishkaandago’Ikwe Health Services and the communities it serves, potentially by improving wound tracking, monitoring and workflow efficiency.

.jpg)