Practice Innovations
(PI-018) A Scoping Review on Smart Bandages with Gas Monitoring Capabilities and a Proposed Machine Learning Protocol for On-device Wound Monitoring
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Kevin Tabatabaei, B.S. – Mayo Clinic Alix School of Medicine; Nessa Aghazadeh Mohandesi, M.D. – Dermatology – Mayo Clinic; Afsaneh Alavi, M.D. – Dermatology – Mayo Clinic
Introduction: The integration of the Internet of Things (IoT) into wound care offers revolutionized management of wounds by enabling real-time diagnostic insights, alerts, and treatment capabilities not previously possible in traditional dressings and hydrogel scaffolds. This scoping review explores the impact of gas-detecting smart bandages, specifically those sensing pulse oxygen saturation (SpO2) and tissue oxygenation (pO2), and their potential to improve patient outcomes. As part of this review, we propose a closed-loop, cloud-based protocol for continually fine-tuning predictive models meant to run locally (on-device) via leveraging device IoT capabilities.
Methods: Three electronic databases were searched for current research on smart bandages with gas monitoring capabilities. Studies within the last 10 years focused on at-home wound monitoring were included, while non-human studies and studies focusing on traditional wound care or smart bandages were excluded.
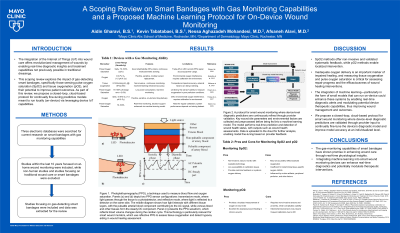
Results: Forty-two studies met the criteria and were included in the scoping review. Both spO2 and pO2 have been demonstrated using well-established methods. SpO2 is primarily measured using photoplethysmography (PPG), with studies testing off-the-shelf PPG modules and custom electrochemical sensors. Electrochemical techniques have shown 1.5 µA/% sensitivity for oxygen monitoring, while optical methods using PPG have successfully measured tissue oxygenation under controlled experimental conditions with an average error of 2.6% (1,2). These methods have proven reliable in static environments such as calibration chambers and simulated settings. Current devices struggle to manage exudate flow, often allowing older exudate to saturate the sensor, hindering the sensor’s ability to capture real-time physiological changes and obtain accurate readings (3,4).
Discussion: The gas-monitoring capabilities of smart bandages have shown promise in enhancing wound care through real-time physiological insights. SpO2 methods offer non-invasive and validated systematic feedback, while pO2 methods enable localized intervention. Inadequate oxygen delivery is an important marker of impaired healing, and measuring tissue oxygenation and pulse oxygen saturation is critical for assessing repair progress and the efficaciousness of wound healing interventions. Moreover, the integration of machine learning—particularly in the form of small models that can run on-device could enhance these systems by enabling real-time diagnostic alerts and modulating potential device therapeutic capabilities, thus improving wound management and outcomes. We propose a closed-loop, cloud-based protocol for smart wound monitoring where device-level diagnostic predictions are validated through provider input to continually fine-tune the device’s diagnostic model and improve model accuracy at an individualized level.
Methods: Three electronic databases were searched for current research on smart bandages with gas monitoring capabilities. Studies within the last 10 years focused on at-home wound monitoring were included, while non-human studies and studies focusing on traditional wound care or smart bandages were excluded.
Results: Forty-two studies met the criteria and were included in the scoping review. Both spO2 and pO2 have been demonstrated using well-established methods. SpO2 is primarily measured using photoplethysmography (PPG), with studies testing off-the-shelf PPG modules and custom electrochemical sensors. Electrochemical techniques have shown 1.5 µA/% sensitivity for oxygen monitoring, while optical methods using PPG have successfully measured tissue oxygenation under controlled experimental conditions with an average error of 2.6% (1,2). These methods have proven reliable in static environments such as calibration chambers and simulated settings. Current devices struggle to manage exudate flow, often allowing older exudate to saturate the sensor, hindering the sensor’s ability to capture real-time physiological changes and obtain accurate readings (3,4).
Discussion: The gas-monitoring capabilities of smart bandages have shown promise in enhancing wound care through real-time physiological insights. SpO2 methods offer non-invasive and validated systematic feedback, while pO2 methods enable localized intervention. Inadequate oxygen delivery is an important marker of impaired healing, and measuring tissue oxygenation and pulse oxygen saturation is critical for assessing repair progress and the efficaciousness of wound healing interventions. Moreover, the integration of machine learning—particularly in the form of small models that can run on-device could enhance these systems by enabling real-time diagnostic alerts and modulating potential device therapeutic capabilities, thus improving wound management and outcomes. We propose a closed-loop, cloud-based protocol for smart wound monitoring where device-level diagnostic predictions are validated through provider input to continually fine-tune the device’s diagnostic model and improve model accuracy at an individualized level.

.jpg)