Clinical Research
(CR-053) Improving Wound Tissue Evaluation Accuracy: Comparing Clinician Assessments and Ai-driven Technology Across Diverse Skin Tones
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Robert D. J. Fraser, MN RN NSWOC WOCC – Vice President Clinical Innovation, Swift Medical Inc.; Sheila Wang, MD,PhD – Women College Hospital; Amy Cassata, BSN, RN, WCC; Justin Allport, BA,MSc
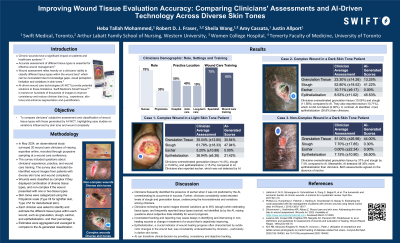
Introduction: Chronic wounds have a significant impact on healthcare worldwide.1 Accurate assessment of wound tissue types such as granulation, slough, eschar, and epithelialization is crucial for effective management.2 However, human evaluations can be inconsistent due to knowledge gaps, visual perception limitations, and variations in skin tone.2 AI-driven wound care technologies (AI-WCT) provide potential solutions to these limitations by offering more objective and reliable assessments.3 This study aimed to compare clinicians' subjective evaluations of wound tissue types with those generated by AI-WCT.
Methods: An observational comparative study was conducted with 20 wound care clinicians recruited at the Nurses Specialized in Wound, Ostomy, and Continence (NSWOC) conference. Participants assessed wound images from patients with diverse skin tones and wound complexities. Clinicians identified and estimated tissue types, which were then compared to AI-WCT assessments. Wounds were classified as complex or non-complex, and skin tones were categorized using the Fitzpatrick scale (Type I/II for light skin, Type V/VI for dark skin). The Chi-square test was used for comparison of categorical variables.
Results:
The study revealed significant discrepancies between clinician and AI assessments. In darker-skinned patients (Fitzpatrick Type V/VI), clinicians overestimated granulation tissue by 10.05%-37% and slough by 7.4%-11.58% (P< 0.001). Epithelialization was underreported by an average of 36.98% compared to the AI-WCT assessments. In contrast, for lighter-skinned patients (Fitzpatrick Type I/II), clinicians overestimated epithelialization by 15.52%.
Additionally, clinicians tended to identify and quantify eschar despite their absence, as indicated by AI. In dark-skinned patients, clinicians overestimated eschar by an average of 10.7%, while in light-skinned patients, clinicians overestimated it by 5.2%. Inconsistencies were less pronounced in the light-skinned patients than in darker-skinned patients.
Discussion:
The findings highlight the challenges clinicians face in evaluating wounds, particularly in darker-skinned patients. AI-based tools offer more consistent, objective measurements and may reduce subjectivity, improving diagnostic accuracy and equity.
Methods: An observational comparative study was conducted with 20 wound care clinicians recruited at the Nurses Specialized in Wound, Ostomy, and Continence (NSWOC) conference. Participants assessed wound images from patients with diverse skin tones and wound complexities. Clinicians identified and estimated tissue types, which were then compared to AI-WCT assessments. Wounds were classified as complex or non-complex, and skin tones were categorized using the Fitzpatrick scale (Type I/II for light skin, Type V/VI for dark skin). The Chi-square test was used for comparison of categorical variables.
Results:
The study revealed significant discrepancies between clinician and AI assessments. In darker-skinned patients (Fitzpatrick Type V/VI), clinicians overestimated granulation tissue by 10.05%-37% and slough by 7.4%-11.58% (P< 0.001). Epithelialization was underreported by an average of 36.98% compared to the AI-WCT assessments. In contrast, for lighter-skinned patients (Fitzpatrick Type I/II), clinicians overestimated epithelialization by 15.52%.
Additionally, clinicians tended to identify and quantify eschar despite their absence, as indicated by AI. In dark-skinned patients, clinicians overestimated eschar by an average of 10.7%, while in light-skinned patients, clinicians overestimated it by 5.2%. Inconsistencies were less pronounced in the light-skinned patients than in darker-skinned patients.
Discussion:
The findings highlight the challenges clinicians face in evaluating wounds, particularly in darker-skinned patients. AI-based tools offer more consistent, objective measurements and may reduce subjectivity, improving diagnostic accuracy and equity.

.jpg)