Case Series/Study
(CS-049) Modified Gips Procedure in the Treatment of Pilonidal Sinus Disease: A Case Series
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Laurel Adams, BS; Jessica Reid, MS; Leely Rezvani, MD, MS; Abigail Chaffin, MD, FACS, CWSP, MAPWCA
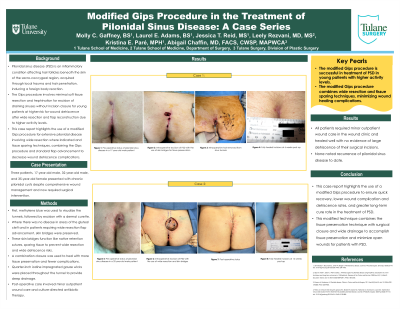
Introduction: Pilonidal sinus disease (PSD) is an inflammatory condition affecting hair follicles beneath the skin of the sacro-coccygeal region. PSD is acquired through local trauma and hair penetration, inducing a foreign body reaction. The Gips procedure is published in pediatric surgery literature as a preferred technique for management of PSD involving minimal soft tissue resection and trephination for excision of draining sinuses without incision closure for young patients at higher risk for wound dehiscence after wide resection and flap reconstruction due to higher activity levels. This case report highlights the use of a modified Gips procedure for extensive pilonidal disease with wide resection where indicated and tissue sparing techniques, combining the Gips procedure and standard flap advancement to decrease wound dehiscence complications.
Methods: Three patients, 17-year-old male, 35-year-old female, and 32-year-old male, presented with chronic pilonidal cysts despite comprehensive wound management and now required surgical intervention. A modified Gips procedure was created to perform tissue sparing with less wide resection and flap advancement to decrease wound complications. First, methylene blue was used to visualize the tunnels, followed by excision with a dermal curette. Where there was no disease in areas of the gluteal cleft and in patients requiring wide resection flap advancement, skin bridges were preserved. These skin bridges function like native retention sutures, sparing tissue to prevent wide resection and wide dehiscence risks. A combination closure was used to heal with more tissue preservation and fewer complications, and quarter-inch iodoform wicks were placed throughout the tunnel to provide deep drainage. Post-operative care involved minor outpatient wound care and culture-directed antibiotic therapy.
Results: All patients required minor outpatient wound care in the wound clinic and healed well with no evidence of large dehiscence of their surgical incisions. None noted recurrence of pilonidal sinus disease to date.
Discussion: This case report highlights the use of a modified Gips procedure to ensure quick recovery, lower wound complication and dehiscence rates, and greater long-term cure rate in the treatment of PSD. This modified technique combines the tissue preservation technique with surgical closure and wide drainage to accomplish tissue preservation and minimize open wounds for patients with PSD.
Methods: Three patients, 17-year-old male, 35-year-old female, and 32-year-old male, presented with chronic pilonidal cysts despite comprehensive wound management and now required surgical intervention. A modified Gips procedure was created to perform tissue sparing with less wide resection and flap advancement to decrease wound complications. First, methylene blue was used to visualize the tunnels, followed by excision with a dermal curette. Where there was no disease in areas of the gluteal cleft and in patients requiring wide resection flap advancement, skin bridges were preserved. These skin bridges function like native retention sutures, sparing tissue to prevent wide resection and wide dehiscence risks. A combination closure was used to heal with more tissue preservation and fewer complications, and quarter-inch iodoform wicks were placed throughout the tunnel to provide deep drainage. Post-operative care involved minor outpatient wound care and culture-directed antibiotic therapy.
Results: All patients required minor outpatient wound care in the wound clinic and healed well with no evidence of large dehiscence of their surgical incisions. None noted recurrence of pilonidal sinus disease to date.
Discussion: This case report highlights the use of a modified Gips procedure to ensure quick recovery, lower wound complication and dehiscence rates, and greater long-term cure rate in the treatment of PSD. This modified technique combines the tissue preservation technique with surgical closure and wide drainage to accomplish tissue preservation and minimize open wounds for patients with PSD.

.jpg)