Clinical Research
(CR-048) Moisture-associated Skin Damage in Hidradenitis Suppurativa: Prevalence, Risk Factors, and Management Strategies
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Bianca Cei, MD – Department of Dermatology – University of Pisa, Pisa, Italy; Giorgia Salvia, MD – Department of Dermatology – University of Pisa, Pisa, Italy; Flavia Manzo Margiotta, MD – Department of Dermatology – University of Pisa, Pisa, Italy; Antonella Vietina, MD – Department of Dermatology – University of Pisa, Pisa, Italy; Valentina Dini, MD, PhD – Department of Dermatology – University of Pisa, Pisa, Italy; Marco Romanelli, MD, PhD – Department of Dermatology – University of Pisa, Pisa, Italy
Introduction: Hidradenitis suppurativa (HS) is a chronic inflammatory skin condition characterized by painful nodules, abscesses and scarring, primarily affecting apocrine gland-bearing areas [1]. The risk of Moisture-Associated Skin Damage (MASD) in patients with HS is significant due to persistent moisture from sweat, exudate from lesions, and chronic inflammation. This study aims to explore a novel type of MASD, specifically associated with HS, focusing on the underlying mechanisms, clinical implications and management strategies.
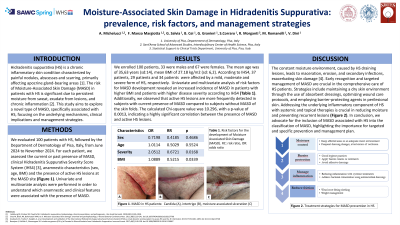
Methods: We evaluated 100 patients with HS, followed by the Department of Dermatology of Pisa, Italy, from June 2024 to November 2024. For each patient, we assessed the current or past presence of MASD, clinical Hidradenitis Suppurativa Severity Score System (IHS4) [2], anamnestic characteristics (sex, age, BMI) and the presence of active HS lesions at the MASD site. Univariate and multivariate analysis were performed in order to understand which anamnestic and clinical features were associated with the presence of MASD.
Results: We enrolled 100 patients, 33 were males and 67 were females. The mean age was of 35,63 years (sd:14), mean BMI of 27.18 kg/m2 (sd: 6,2). According to IHS4, 37 patients, 29 patients and 34 patients were affected by a mild, moderate and severe form of HS, respectively. Univariate and multivariate analysis of risk factors for MASD development revealed an increased incidence of MASD in patients with higher BMI (OR: 1.09, p value: 0.03) and patients with higher disease severity according to IHS4 (OR: 2.05 p value: 0.016). Additionally, we observed that active HS lesions are more frequently detected in subjects with current presence of MASD compared to subjects without MASD of the skin folds. The calculated Chi-square value was 10.296, with a p-value of 0.0013, indicating a highly significant correlation between the presence of MASD and active HS lesions.
Discussion: The constant moisture environment, caused by HS draining lesions, leads to maceration, erosion, and secondary infections, exacerbating skin damage [3]. Early recognition and targeted management of MASD are crucial in the comprehensive care of HS patients. Strategies include maintaining a dry skin environment through the use of absorbent dressings, optimizing wound care protocols, and employing barrier-protecting agents in perilesional skin [4]. Addressing the underlying inflammatory component of HS with systemic and topical therapies is crucial in reducing moisture and preventing recurrent lesions. In conclusion we advocate for the inclusion of MASD associated with HS into the classification of MASD, highlighting the importance for targeted and specific prevention and management plan.
Methods: We evaluated 100 patients with HS, followed by the Department of Dermatology of Pisa, Italy, from June 2024 to November 2024. For each patient, we assessed the current or past presence of MASD, clinical Hidradenitis Suppurativa Severity Score System (IHS4) [2], anamnestic characteristics (sex, age, BMI) and the presence of active HS lesions at the MASD site. Univariate and multivariate analysis were performed in order to understand which anamnestic and clinical features were associated with the presence of MASD.
Results: We enrolled 100 patients, 33 were males and 67 were females. The mean age was of 35,63 years (sd:14), mean BMI of 27.18 kg/m2 (sd: 6,2). According to IHS4, 37 patients, 29 patients and 34 patients were affected by a mild, moderate and severe form of HS, respectively. Univariate and multivariate analysis of risk factors for MASD development revealed an increased incidence of MASD in patients with higher BMI (OR: 1.09, p value: 0.03) and patients with higher disease severity according to IHS4 (OR: 2.05 p value: 0.016). Additionally, we observed that active HS lesions are more frequently detected in subjects with current presence of MASD compared to subjects without MASD of the skin folds. The calculated Chi-square value was 10.296, with a p-value of 0.0013, indicating a highly significant correlation between the presence of MASD and active HS lesions.
Discussion: The constant moisture environment, caused by HS draining lesions, leads to maceration, erosion, and secondary infections, exacerbating skin damage [3]. Early recognition and targeted management of MASD are crucial in the comprehensive care of HS patients. Strategies include maintaining a dry skin environment through the use of absorbent dressings, optimizing wound care protocols, and employing barrier-protecting agents in perilesional skin [4]. Addressing the underlying inflammatory component of HS with systemic and topical therapies is crucial in reducing moisture and preventing recurrent lesions. In conclusion we advocate for the inclusion of MASD associated with HS into the classification of MASD, highlighting the importance for targeted and specific prevention and management plan.

.jpg)