Case Series/Study
(CS-029) Multistate Model of Lower-extremity Chronic Wounds, Amputations, and Mortality: Retrospective Cohort Study of a Statewide Patient Registry
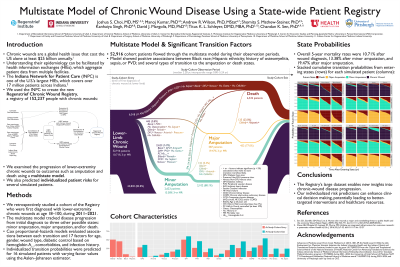
Chronic wounds are a global health issue that cost the US alone at least $25 billion annually. Understanding their epidemiology can be facilitated by health information exchanges (HIEs), which aggregate patient data from multiple facilities. We created a new chronic-wound patient registry from one of the U.S.’s largest HIEs, which combines patient records from over 18,000 outpatient clinics and more than 90% of hospitals in Indiana, insurance providers, and Indiana’s death registry, covering over 17 million patients. This study examines the progression of lower-extremity chronic wounds to outcomes such as amputation and death using a multistate model. We also predicted individualized patient risk for several simulated patients.
Methods:
We retrospectively examined a cohort of 52,916 patients who were first diagnosed with lower-extremity chronic wounds during 2011–2021. A multistate model tracked disease progression from initial diagnosis to minor amputation, major amputation, and/or death. Cox proportional-hazards models evaluated associations between each state transition and 17 covariates.
Results:
Three-year mortality rates in the cohort were 10.71% after first wound diagnosis, 13.38% after minor amputation, and 19.47% after major amputation. The multistate model revealed significant associations between several events and covariates: Black race with increased amputation, Hispanic ethnicity with increased death before amputation, peripheral vascular disease with increased amputation and increased death before amputation, osteomyelitis with increased amputation and decreased death before amputation or after minor amputation, and sepsis with increased death before amputation or after minor amputation. Individualized risks were estimated for several simulated patients: e.g., the probability of major amputation, within three years after minor amputation, was respectively 6.0% and 16.7% for White and Black patients who are non-Hispanic and diabetic.
Discussion:
The state-wide patient registry’s large, diverse dataset enables new insights into chronic-wound progression and associated risks. By identifying key factors associated with amputation and death, including disparities between race and ethnicity categories, the research highlights the need for personalized care strategies. The individualized risk predictions from this study’s multistate model can enhance clinical decision making, potentially improving patient management. These insights could lead to better-targeted interventions and more effective use of healthcare resources in treating chronic wounds.

.jpg)