Clinical Research
(CR-034) Predicting Discharge Walking Ability in Diabetic Foot Ulcer Patients Using Machine Learning
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Kenichi Kono, Ph.D – Associate professor, International University of Health and Welfare; Kazuki Kimura, Ph.D – Associate professor, Niigata University of Rehabilitation; Shinsuke Imaoka, Ph.D – Oita Oka Hospital; Naoya Oseki, Ph.D – Tokyo Medical University Ibaraki Medical Center; Nobuhide Kawabe, Ph.D – Professor, Tohto University
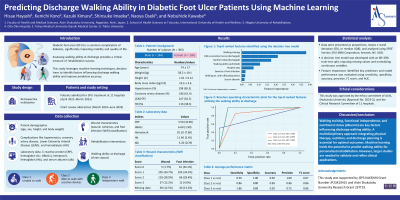
Introduction: Diabetic foot ulcer (DFU) are a common complication of diabetes, significantly impacting mobility and quality of life. Assessing walking ability at discharge provides a critical measure for rehabilitation success. This study leverages machine learning techniques, decision trees to identify factors influencing discharge walking ability and improve predictive accuracy.
Methods: A retrospective investigation examined 303 patients admitted for DFU treatment from April 2021 to March 2023. The study collected data on various factors, including demographic characteristics (such as age and gender), clinical parameters (such as albumin and HbA1c levels), comorbidities (including neuropathy and ischemia), wound characteristics (such as location and infection severity), and rehabilitation interventions (encompassing gait training and activities of daily living exercises). Walking ability at discharge, the primary outcome, was categorized into three classes consistent with the results: Class 1: Unable to walk, Class 2: Able to walk with assistive devices, Class 3: Independent walking. A decision tree model was developed using an 80-20% train-test split. Missing values were imputed, and continuous variables were normalized. Model performance was evaluated using accuracy, F1-score, and area under the curve (AUC). Feature importance was analyzed to identify key predictors.
Results: "Walking training content" was identified as the most influential factor, followed by "walking ability FIM score at discharge," "ADL_BI score at discharge," and "baseline walking ability." Intensive walking training and higher FIM scores were associated with independent walking. Shorter hospital stays benefited patients with higher initial walking capacity. The model achieved an accuracy of 80.3%, an F1-score of 79.5%, and a macro-average AUC of 0.894. Class-specific AUCs were 0.916 for Class 1 (unable to walk), 0.852 for Class 2 (walking with assistive devices), and 0.916 for Class 3 (independent walking).
Discussion: Focused rehabilitation strategies, including walking training and functional independence improvements, are crucial for enhancing discharge walking ability. Nutritional status, reflected by albumin levels, further influences outcomes. A multidisciplinary approach integrating physical therapy, nutritional support, and individualized discharge planning is essential. Machine learning provides a reliable framework for predicting walking ability, supporting data-driven, personalized rehabilitation strategies. Future studies should validate these findings in larger cohorts to refine clinical applications.
Methods: A retrospective investigation examined 303 patients admitted for DFU treatment from April 2021 to March 2023. The study collected data on various factors, including demographic characteristics (such as age and gender), clinical parameters (such as albumin and HbA1c levels), comorbidities (including neuropathy and ischemia), wound characteristics (such as location and infection severity), and rehabilitation interventions (encompassing gait training and activities of daily living exercises). Walking ability at discharge, the primary outcome, was categorized into three classes consistent with the results: Class 1: Unable to walk, Class 2: Able to walk with assistive devices, Class 3: Independent walking. A decision tree model was developed using an 80-20% train-test split. Missing values were imputed, and continuous variables were normalized. Model performance was evaluated using accuracy, F1-score, and area under the curve (AUC). Feature importance was analyzed to identify key predictors.
Results: "Walking training content" was identified as the most influential factor, followed by "walking ability FIM score at discharge," "ADL_BI score at discharge," and "baseline walking ability." Intensive walking training and higher FIM scores were associated with independent walking. Shorter hospital stays benefited patients with higher initial walking capacity. The model achieved an accuracy of 80.3%, an F1-score of 79.5%, and a macro-average AUC of 0.894. Class-specific AUCs were 0.916 for Class 1 (unable to walk), 0.852 for Class 2 (walking with assistive devices), and 0.916 for Class 3 (independent walking).
Discussion: Focused rehabilitation strategies, including walking training and functional independence improvements, are crucial for enhancing discharge walking ability. Nutritional status, reflected by albumin levels, further influences outcomes. A multidisciplinary approach integrating physical therapy, nutritional support, and individualized discharge planning is essential. Machine learning provides a reliable framework for predicting walking ability, supporting data-driven, personalized rehabilitation strategies. Future studies should validate these findings in larger cohorts to refine clinical applications.

.jpg)