Case Series/Study
(CS-005) Preoperative Wound Bed Preparation Using Fluorescence Imaging to Optimize Outcomes in Chronic Wound Reconstruction
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Michael Desvigne, MD FACS; Arti Kamur, DPM
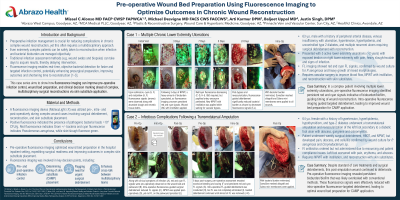
Introduction: Preoperative infection management is crucial for reducing complications in chronic wound reconstruction. Traditional infection assessment methods can delay intervention (e.g., microbiology). Fluorescence wound imaging* enables real-time, objective bacterial detection for faster and targeted infection control, potentially enhancing presurgical preparation, improving outcomes and shortening time to reconstruction. This study aims to evaluate the impact of preoperative fluorescence imaging in optimizing wound bed preparation ahead of complex reconstructions via grafts and flaps.
Methods: Ten candidates for chronic wound surgical reconstruction via grafting (autologous or skin substitutes) (pressure injuries, diabetic foot ulcers, venous leg ulcers, and non-healing surgical wounds) were evaluated using fluorescence imaging during their preoperative hospital stay. The imaging assessed the location and presence of bacteria at pathologic loads (≥10⁴ CFU/gr) in both the wound and surrounding tissue. Based on the fluorescence imaging findings, targeted wound debridement, cleansing, and antibiotic therapy were employed to manage infection and reduce bacterial load prior to surgery, with the goal of eliminating or significantly reducing fluorescence signals. Postoperative outcomes, including healing time, infection rates, and complications, are described.
Results: Fluorescence imaging revealed bacterial contamination and biofilm in all 10 cases, guiding additional debridement and more precise antibiotic therapy prior to reconstructive surgery. The treatment algorithm, as guided by fluorescence, included mechanical debridement, surgical debridement, and negative pressure wound therapy (NPWT) with or without installation. Antibiotic therapy was initiated for any patient showing evidence of acute infection. Fluorescence imaging was involved in key decision points, including: 1) preoperative infection control, 2) urgent surgical debridement, 3) timing of surgical closure.
Discussion: Preoperative fluorescence imaging optimized wound bed preparation in the hospital inpatient setting, expediting surgical readiness and improving outcomes in complex autologous skin or biologic skin substitute placement. It provided real-time, objective insights into bacterial load, enabling targeted infection control, faster healing, and fewer complications.
Methods: Ten candidates for chronic wound surgical reconstruction via grafting (autologous or skin substitutes) (pressure injuries, diabetic foot ulcers, venous leg ulcers, and non-healing surgical wounds) were evaluated using fluorescence imaging during their preoperative hospital stay. The imaging assessed the location and presence of bacteria at pathologic loads (≥10⁴ CFU/gr) in both the wound and surrounding tissue. Based on the fluorescence imaging findings, targeted wound debridement, cleansing, and antibiotic therapy were employed to manage infection and reduce bacterial load prior to surgery, with the goal of eliminating or significantly reducing fluorescence signals. Postoperative outcomes, including healing time, infection rates, and complications, are described.
Results: Fluorescence imaging revealed bacterial contamination and biofilm in all 10 cases, guiding additional debridement and more precise antibiotic therapy prior to reconstructive surgery. The treatment algorithm, as guided by fluorescence, included mechanical debridement, surgical debridement, and negative pressure wound therapy (NPWT) with or without installation. Antibiotic therapy was initiated for any patient showing evidence of acute infection. Fluorescence imaging was involved in key decision points, including: 1) preoperative infection control, 2) urgent surgical debridement, 3) timing of surgical closure.
Discussion: Preoperative fluorescence imaging optimized wound bed preparation in the hospital inpatient setting, expediting surgical readiness and improving outcomes in complex autologous skin or biologic skin substitute placement. It provided real-time, objective insights into bacterial load, enabling targeted infection control, faster healing, and fewer complications.

.jpg)