Practice Innovations
(PI-010) Preoperative Wound Bed Preparation Using Fluorescence Imaging to Optimize Outcomes in Complex Wound Management and Reconstruction
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Misael Alonso, MD, FACP, CWSP, FAPWCA
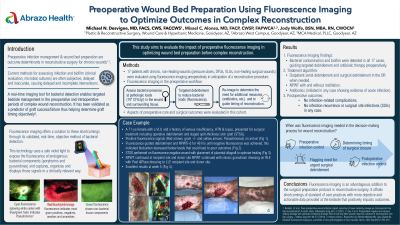
Introduction: Preoperative infection management and wound bed preparation is a critical step in reducing postoperative complications and improving outcomes in reconstructive surgery for chronic wounds. Methods of assessing bacterial infection and biofilm presence such as clinical evaluation and microbial cultures are often subjective, inaccurate and can delay necessary interventions. Fluorescence imaging technology (MolecuLight®), provides real-time, objective detection of bacterial presence in wounds, enabling targeted management of infection and biofilm. This study aims to evaluate the impact of preoperative fluorescence imaging in assessing and optimizing wound bed preparation prior to complex reconstruction.
Methods: A total of seventeen (n=17) patients with chronic, non-healing wounds (pressure ulcers, DFUs, VLUs, and non-healing surgical wounds) were evaluated preoperatively using fluorescence imaging to assess location and presence of bacteria at pathologic loads (104 CFU/gr) in the wound and surrounding tissue. Based on fluorescence imaging findings, targeted wound debridement, cleansing, and antibiotic therapy were initiated to reduce bacterial load prior to surgery until fluorescence signals were eradicated or significantly reduced. In some cases, the need for operative debridement was in part determined by the imaging results. Postoperative outcomes, including healing time, infection rates, and complications, were compared to historical data from similar cases managed with standard care methods. In addition, objective imaging served as a tool to assist with management decisions.
Results: Fluorescence imaging revealed bacterial contamination and biofilm in 17 of the 17 cases, guiding additional debridement and more precise antibiotic therapy prior to surgery. The treatment algorithm as guided by fluorescence included: office and bed side debridement, surgical debridement, negative pressure wound therapy (NPWT) with and without instillation. Antibiotic therapy was initiated in any patient revealing evidence of acute infection. Segments of the management protocol where fluorescence imaging was involved in the decision-making process typically involved: 1) Preoperative infection control, 2) Urgent surgical debridement, 3) Timing of surgical closure, and 4) Postoperative infection control. Postoperative healing occurred without infection-related complications in all surgical cases. No patients experienced infection recurrence or surgical site infections (SSIs).
Discussion: The preoperative use of fluorescence imaging for wound bed preparation significantly enhanced surgical outcomes in complex skin reconstruction. Additionally, fluorescence imaging proved valuable in guiding management decisions. By offering real-time, objective insights into bacterial load and biofilm presence, it enables more targeted and effective infection control, ultimately leading to faster healing and fewer postoperative complications.
Methods: A total of seventeen (n=17) patients with chronic, non-healing wounds (pressure ulcers, DFUs, VLUs, and non-healing surgical wounds) were evaluated preoperatively using fluorescence imaging to assess location and presence of bacteria at pathologic loads (104 CFU/gr) in the wound and surrounding tissue. Based on fluorescence imaging findings, targeted wound debridement, cleansing, and antibiotic therapy were initiated to reduce bacterial load prior to surgery until fluorescence signals were eradicated or significantly reduced. In some cases, the need for operative debridement was in part determined by the imaging results. Postoperative outcomes, including healing time, infection rates, and complications, were compared to historical data from similar cases managed with standard care methods. In addition, objective imaging served as a tool to assist with management decisions.
Results: Fluorescence imaging revealed bacterial contamination and biofilm in 17 of the 17 cases, guiding additional debridement and more precise antibiotic therapy prior to surgery. The treatment algorithm as guided by fluorescence included: office and bed side debridement, surgical debridement, negative pressure wound therapy (NPWT) with and without instillation. Antibiotic therapy was initiated in any patient revealing evidence of acute infection. Segments of the management protocol where fluorescence imaging was involved in the decision-making process typically involved: 1) Preoperative infection control, 2) Urgent surgical debridement, 3) Timing of surgical closure, and 4) Postoperative infection control. Postoperative healing occurred without infection-related complications in all surgical cases. No patients experienced infection recurrence or surgical site infections (SSIs).
Discussion: The preoperative use of fluorescence imaging for wound bed preparation significantly enhanced surgical outcomes in complex skin reconstruction. Additionally, fluorescence imaging proved valuable in guiding management decisions. By offering real-time, objective insights into bacterial load and biofilm presence, it enables more targeted and effective infection control, ultimately leading to faster healing and fewer postoperative complications.

.jpg)