Case Series/Study
(CS-136) Pressure Ulcer with Exposed Tendon Heals After Five Applications of a Novel Biomimetic Matrix: A Case Study
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Introduction: Wounds with exposed structures are challenging due to slow healing and high rates of infection and complications. Treatment of complex lower-extremity wounds requires a multifaceted approach including aggressive debridement, moist wound care, blood flow optimization, bioburden reduction, and often flap reconstruction1. Given that flap reconstruction is implausible in high-risk patients, it is critical to find alternative modalities that encourage rapid granulation over the exposed structures and achieve wound closure1. This case report describes the use of a novel biomimetic matrix (BMM) to treat a pressure ulcer with exposed tendon in a patient with numerous comorbidities. BMM is designed to support healing of complex wounds by providing an acellular 3D scaffold for tissue regrowth, with antibacterial protection, delivered via a syringe-based system for precise placement and dead space elimination.
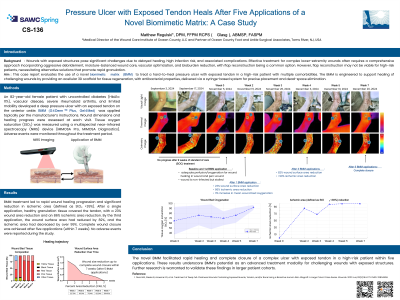
Methods: The patient was an 82-year-old female with uncontrolled diabetes (HbA1c: 11%), vascular disease, severe rheumatoid arthritis, and reduced mobility. She developed a deep pressure ulcer with exposed tendon in the anterior ankle. BMM* was applied topically per the manufacturer’s instructions. Wound measurements were recorded at baseline and at each following visit. Tissue oxygen saturation (StO₂) was assessed using a multispectral near-infrared spectroscopy (NIRS) imaging device**. Adverse events were monitored throughout the study.
Results: BMM treatment resulted in rapid wound healing progression and ischemic area [defined as StO₂ < 39%] reduction. After a single application, there was substantial wound depth reduction with healthy granulation tissue covering the tendon, accompanied by 23% wound area reduction and 86% ischemic area reduction. Within 4 BMM applications, 82% wound surface area reduction and >99% ischemic area reduction was achieved, resulting in complete wound closure after 5 applications. No adverse events were observed during the study period.
Discussion: BMM successfully facilitated healing of a complex ulcer with exposed tendon in a patient with several risk factors, achieving complete wound closure with just five applications. These findings highlight BMM’s potential for rapid healing progression in complex wounds with exposed structures, suggesting an advanced alternative modality. Further studies are necessary to confirm these results and evaluate BMM’s performance in a larger patient population.
Methods: The patient was an 82-year-old female with uncontrolled diabetes (HbA1c: 11%), vascular disease, severe rheumatoid arthritis, and reduced mobility. She developed a deep pressure ulcer with exposed tendon in the anterior ankle. BMM* was applied topically per the manufacturer’s instructions. Wound measurements were recorded at baseline and at each following visit. Tissue oxygen saturation (StO₂) was assessed using a multispectral near-infrared spectroscopy (NIRS) imaging device**. Adverse events were monitored throughout the study.
Results: BMM treatment resulted in rapid wound healing progression and ischemic area [defined as StO₂ < 39%] reduction. After a single application, there was substantial wound depth reduction with healthy granulation tissue covering the tendon, accompanied by 23% wound area reduction and 86% ischemic area reduction. Within 4 BMM applications, 82% wound surface area reduction and >99% ischemic area reduction was achieved, resulting in complete wound closure after 5 applications. No adverse events were observed during the study period.
Discussion: BMM successfully facilitated healing of a complex ulcer with exposed tendon in a patient with several risk factors, achieving complete wound closure with just five applications. These findings highlight BMM’s potential for rapid healing progression in complex wounds with exposed structures, suggesting an advanced alternative modality. Further studies are necessary to confirm these results and evaluate BMM’s performance in a larger patient population.

.jpg)