Clinical Research
(CR-033) Speed and Efficiency: Advancing Mobile PAD Assessment with Digital Volume Plethysmography
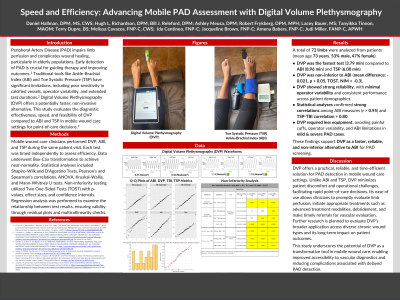
Peripheral Artery Disease (PAD) impairs limb perfusion and complicates wound healing, particularly in elderly populations. Early detection of PAD is crucial for guiding therapy and improving outcomes. Traditional tools like the Ankle-Brachial Index (ABI) and Toe Systolic Pressure (TSP) have significant limitations, including poor sensitivity in calcified vessels, operator variability, and extended test durations. Digital Volume Plethysmography (DVP*) offers a faster, non-invasive alternative. This study evaluates the effectiveness, speed, and feasibility of DVP compared to ABI and TSP in mobile wound care settings for point-of-care decisions.
Methods:
Mobile wound care clinicians performed DVP, ABI, and TSP during the same patient visit. Tests were timed independently to assess efficiency. Data underwent Box-Cox transformation to achieve near-normality. Statistical analyses included Shapiro-Wilk and D'Agostino tests, Pearson's and Spearman's correlations, ANOVA, Kruskal-Wallis, and Mann-Whitney U tests. Non-inferiority testing utilized Two One-Sided Tests (TOST) with p-values, effect sizes, and confidence intervals. Regression analysis was performed to examine the relationship between test results, ensuring validity through residual plots and multicollinearity checks.
Results:
N=51 participants (95 extremities) with an average age of 72. DVP consistently demonstrated faster completion times (mean: 3.79 minutes) compared to ABI (mean: 8.96 minutes) and TSP (mean: 6.00 minutes). DVP was non-inferior to ABI, with a mean difference of -0.021 (p < 0.05 for the lower bound TOST). The DVP method had fewer limitations, required less specialized equipment, and avoided issues such as painful cuffs, poor sensitivity for mild PAD, operator variability, and severe PAD challenges.
Discussion:
DVP offers a practical, reliable, and time-efficient solution for PAD detection in mobile wound care settings. Unlike ABI and TSP, DVP minimizes patient discomfort and operational challenges, facilitating rapid point-of-care decisions. Its ease of use allows clinicians to promptly evaluate limb perfusion, initiate appropriate treatments—such as debridement and biologics—and make timely referrals for vascular evaluation. Further research is planned to evaluate DVP’s broader application across diverse chronic wound types and its long-term impact on patient outcomes.
This study underscores the potential of DVP as a transformative tool in mobile wound care, enabling improved accessibility to vascular assessments and reducing complications associated with delayed PAD detection.

.jpg)