Case Series/Study
(CS-159) Successful Fish Skin Xenograft Reconstruction of a Complex Scalp Wound with Exposed Cranium Secondary to Gorlin Syndrome
Gorlin syndrome or Nevoid Basal Cell Carcinoma syndrome is an autosomal dominant familial cancer syndrome which may cause hundreds of basal cells over a patient's lifetime. It is characterized by a triad of manifestations to include multiple basal cell cancers, odontogenic keratocysts and skeletal deformities. Palmar and plantar skin pitting is also common. Prevalence is estimated at 1 per 40,000-60,000. The disease affects men and women equally. Patients can develop basal cell cancers as early as infancy with the median age being 20 years. It is caused by a mutation in patched 1 (PTCH), a tumor suppressor gene located on chromosome 9q. This gene encodes a transmembrane receptor protein that recognizes signaling proteins of the sonic hedgehog family. Activation of this mutated gene leads to tumorgenicity.1,2,3 This case report highlights the clinical efficacy of fish skin xenografts in this unique subset of rare patients.
Methods:
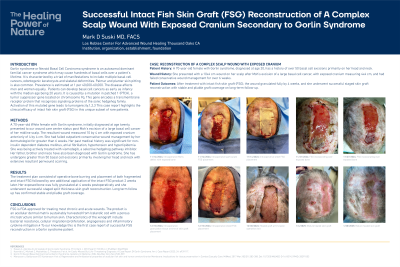
A 70 year old White female with Gorlin syndrome, initially diagnosed at age twenty, presented to our wound care center status post Moh’s excision of a large basal cell cancer of her midline scalp. The resultant wound measured 10 by 4 cm with exposed cranium anteriorly of 4 by 4 cm. She had failed outpatient conservative wound management by her dermatologist for greater than 6 weeks. Her past medical history was significant for non-insulin dependent diabetes mellitus, atrial fibrillation, hypertension and hyperlipidemia. She was being actively treated with vismodegib, a selective hedgehog pathway inhibitor. Her father, brother and niece have also been diagnosed with Gorlin syndrome. She has undergone greater than 50 basal cell excisions primarily involving her head and neck with extensive resultant periwound scarring.
Results:
The treatment plan consisted of operative bone burring and placement of both particulate and sheet fish skin xenografts followed by one additional application of the sheet product 2 weeks later. Her exposed bone was fully granulated at 4 weeks postoperatively and she underwent successful staged split thickness skin graft reconstruction. Long term follow up has confirmed stable and pliable graft coverage.
Discussion:
Fish skin xenografts are FDA approved for treating most chronic and acute wounds. The product is an acellular dermal matrix sustainably harvested from Icelandic cod with a porous microstructure similar to human skin. Characteristics of the xenograft include bacterial resistance, cellular migration/proliferation, angiogenesis and inflammatory cytokine mitigation.4 To our knowledge this is the first case report of successful fish skin xenograft reconstruction in a Gorlin syndrome patient.

.jpg)