Case Series/Study
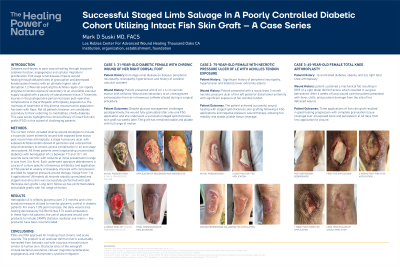
(CS-158) Successful Staged Limb Salvage in a Poorly Controlled Diverse Diabetic Cohort Utilizing Fish Skin Xenografts– a Case Series
Diabetes contributes to poor wound healing through impaired cytokine function, angiogenesis and cellular migration/proliferation. End stage renal disease impairs wound healing through delayed rates of granulation and decreased keratinization kinetics with an ultimate higher rate of disruption.1,2 Wounds overlying the Achilles region can rapidly progress to tendon exposure secondary to an unreliable vascular supply coupled with a paucity of subcutaneous tissue.3 Traumatic injuries in the postoperative period increases post-operative complications in the orthopedic arthroplasty population.4 The mainstay of treatment of this diverse reconstructive population has been with flaps. Not all patients however are candidates secondary to their underling co-morbidities, chiefly diabetes. This case series highlights the clinical efficacy of fish skin xenografts in this subset of challenging patients.
Methods:
The current cohort included diverse wound etiologies to include a traumatic lower extremity wound with exposed bone status post recent knee arthroplasty, a stage 4 pressure ulcer with exposed Achilles tendon devoid of peritenon and a dorsal foot wound secondary to venous access complication in an end stage renal patient. All three patients were longstanding uncontrolled diabetics with hemoglobin A1c’s between 7.5 and 10.1. All wounds were necrotic with cellulitis at initial presentation. ( range in size from 3 to 8cm)
Each underwent operative debridement, a course of culture specific intravenous antibiotics and application of fish skin xenografts placed at weekly or biweekly intervals with compression provided by negative pressure wound therapy. (range from 1 to 6 applications)
Ultimately all wounds robustly granulated and staged reconstruction was successfully performed with split thickness skin grafts. Long term follow up has confirmed stable and pliable grafts with full range of motion.
Results:
Hemoglobin A1c reflects glycemia over 2-3 months and is the standard measure utilized to monitor glycemic control in diabetic patients. For every 1.0% point increase, the daily wound area healing decreases by 0.028cm2/day.5 To avoid amputation in these high risk patients, the use of advanced wound care products to include CAMPS ( Cellular, acellular and matrix – like products) have been recommended.
Discussion:
Fish skin xenografts are FDA approved for treating most chronic and acute wounds. The product is an acellular dermal matrix sustainably harvested from Icelandic cod with a porous microstructure similar to human skin. Characteristics of the xenograft include bacterial resistance, cellular migration/proliferation , angiogenesis an inflammatory cytokine mitigation.

.jpg)