Case Series/Study
(CS-096) The Impact of Moist Wound Dressings on Quality of Life in Patients with Hidradenitis Suppurativa
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Bianca Cei, MD – Department of Dermatology – University of Pisa, Pisa, Italy; Simone Sturli, MD – Department of Dermatology – University of Pisa, Pisa, Italy; Antonella Vietina, MD – Department of Dermatology – University of Pisa, Pisa, Italy; Agata Janowska, MD – Department of Dermatology – University of Pisa, Pisa, Italy; Valentina Dini, MD, PhD – Department of Dermatology – University of Pisa, Pisa, Italy; Marco Romanelli, MD, PhD – Department of Dermatology – University of Pisa, Pisa, Italy
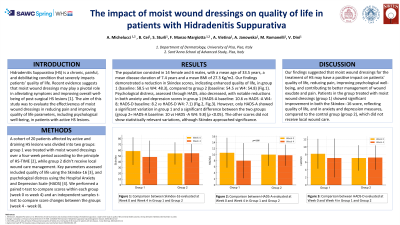
Introduction: Hidradenitis Suppurativa (HS) is a chronic, painful, and debilitating condition that severely impacts patients’ quality of life. Recent evidence suggests that moist wound dressings may play a pivotal role in alleviating symptoms and improving overall well-being of post-surgical HS lesions [1]. The aim of this study was to evaluate the effectiveness of moist wound dressings in reducing pain and improving quality of life parameters, including psychological well-being, in patients with active HS lesions.
Methods: A cohort of 20 patients affected by active and draining HS lesions was divided into two groups: group 1 was treated with moist wound dressings over a four-week period according to the principle of HS-TIME [2], while group 2 didn’t receive local wound care management. Key parameters assessed included quality of life using the Skindex score, and psychological distress using the Hospital Anxiety and Depression Scale (HADS). Baseline and week-four measurements were compared to evaluate outcomes.
Results: The population consists in 14 female and 6 males, with a mean age of 33.5 years, a mean disease duration of 7.4 years and a mean BMI of 27.3 Kg/m2. Our findings demonstrate a reduction in Skindex scores, indicating enhanced quality of life, in group 1 (baseline: 58.5 vs W4: 51.44), when compared to group 2 (baseline: 54.5 vs W4: 54.8). Psychological distress, assessed through HADS, also decreased, with notable reductions in both anxiety and depression scores in group 1 (HADS-A baseline: 10.6 vs HADS -A W4:8; HADS-D baseline: 8.2 vs HADS-D W4:7.4) compared to group 2. Additionally, improvements were observed in wound exudate and pain management.
Discussion: Our findings suggested that moist wound dressings for the treatment of HS may have a positive impact on patients' quality of life, reducing pain, improving psychological well-being, and contributing to better management of wound exudate and pain. Patients in the group treated with moist wound dressings (group 1) showed significant improvement in both the Skindex score, reflecting quality of life, and in anxiety and depression measures, compared to the control group (group 2), which did not receive local wound care.
Methods: A cohort of 20 patients affected by active and draining HS lesions was divided into two groups: group 1 was treated with moist wound dressings over a four-week period according to the principle of HS-TIME [2], while group 2 didn’t receive local wound care management. Key parameters assessed included quality of life using the Skindex score, and psychological distress using the Hospital Anxiety and Depression Scale (HADS). Baseline and week-four measurements were compared to evaluate outcomes.
Results: The population consists in 14 female and 6 males, with a mean age of 33.5 years, a mean disease duration of 7.4 years and a mean BMI of 27.3 Kg/m2. Our findings demonstrate a reduction in Skindex scores, indicating enhanced quality of life, in group 1 (baseline: 58.5 vs W4: 51.44), when compared to group 2 (baseline: 54.5 vs W4: 54.8). Psychological distress, assessed through HADS, also decreased, with notable reductions in both anxiety and depression scores in group 1 (HADS-A baseline: 10.6 vs HADS -A W4:8; HADS-D baseline: 8.2 vs HADS-D W4:7.4) compared to group 2. Additionally, improvements were observed in wound exudate and pain management.
Discussion: Our findings suggested that moist wound dressings for the treatment of HS may have a positive impact on patients' quality of life, reducing pain, improving psychological well-being, and contributing to better management of wound exudate and pain. Patients in the group treated with moist wound dressings (group 1) showed significant improvement in both the Skindex score, reflecting quality of life, and in anxiety and depression measures, compared to the control group (group 2), which did not receive local wound care.

.jpg)