Case Series/Study
(CS-138) The Use of Multiple Modalities for Limb Salvage Due to Severely Infected Wounds: A Case Study
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Laurel Adams, BS; Abigail Chaffin, MD, FACS, CWSP, MAPWCA; Joshua Dickerson, MD; Molly Gaffney, BS
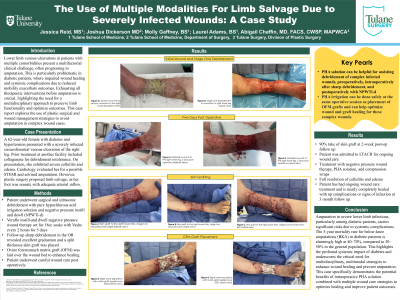
Introduction: Lower limb venous ulcerations in patients with multiple comorbidities present a multifactorial clinical challenge, often unfortunately progressing to amputation. This is particularly problematic in diabetic patients, where impaired wound healing and systemic complications due to reduced mobility exacerbate outcomes. Exhausting all therapeutic interventions before amputation is crucial, highlighting the need for a multidisciplinary approach to preserve limb functionality and optimize outcomes. This case report explores the use of plastic surgical and wound management strategies to avoid amputation in complex wound cases.
Methods: A 62-year-old female with diabetes and hypertension presented with a severely infected circumferential venous ulceration to the right leg. Prior treatment at another outpatient facility included dressing changes with collagenase as she was intolerant to sharp debridement due to pain. On presentation, she exhibited severe cellulitis and edema. Cardiology evaluated her for nSTEMI and additionally evaluated her right leg and advised amputation due to the severity of the venous ulceration and the infection. However, plastic surgery proposed an attempted limb salvage, as her foot was sensate with adequate arterial inflow. She underwent surgical and ultrasonic debridement with HOCl wound irrigation solution, followed by NPWT with instill-and-dwell set for 18 cc soaks with HOCl wound solution every 2 hours for 5 days. Subsequent OR debridement revealed excellent granulation, allowing wound reconstruction with autologous STSG and morselized OFM grafting to enhance wound bed healing.
Results: At 2 weeks post-op, the skin graft achieved 95% take with remaining areas healing well with wound management. The patient, now admitted to LTAC, continues treatment with NPWT, HOCl irrigation, and compression wraps, with full resolution of cellulitis and edema. Daily intensive wound management will ensure optimal healing.
Discussion: Amputation in severe lower limb infections, particularly in diabetic patients, poses significant risks due to systemic complications. The 5-year mortality rate for below-knee amputations (BKA) in diabetic patients is 40–70%, markedly higher than the 30–50% seen in the general population. This underscores the systemic impact of diabetes and the critical need for multidisciplinary, multimodal strategies for limb threatening wounds to promote effective wound healing and avoid amputation.
Methods: A 62-year-old female with diabetes and hypertension presented with a severely infected circumferential venous ulceration to the right leg. Prior treatment at another outpatient facility included dressing changes with collagenase as she was intolerant to sharp debridement due to pain. On presentation, she exhibited severe cellulitis and edema. Cardiology evaluated her for nSTEMI and additionally evaluated her right leg and advised amputation due to the severity of the venous ulceration and the infection. However, plastic surgery proposed an attempted limb salvage, as her foot was sensate with adequate arterial inflow. She underwent surgical and ultrasonic debridement with HOCl wound irrigation solution, followed by NPWT with instill-and-dwell set for 18 cc soaks with HOCl wound solution every 2 hours for 5 days. Subsequent OR debridement revealed excellent granulation, allowing wound reconstruction with autologous STSG and morselized OFM grafting to enhance wound bed healing.
Results: At 2 weeks post-op, the skin graft achieved 95% take with remaining areas healing well with wound management. The patient, now admitted to LTAC, continues treatment with NPWT, HOCl irrigation, and compression wraps, with full resolution of cellulitis and edema. Daily intensive wound management will ensure optimal healing.
Discussion: Amputation in severe lower limb infections, particularly in diabetic patients, poses significant risks due to systemic complications. The 5-year mortality rate for below-knee amputations (BKA) in diabetic patients is 40–70%, markedly higher than the 30–50% seen in the general population. This underscores the systemic impact of diabetes and the critical need for multidisciplinary, multimodal strategies for limb threatening wounds to promote effective wound healing and avoid amputation.

.jpg)