Case Series/Study
(CS-125) Using a Multilayered Leukocyte, Platelet, Fibrin Patch to Cover Exposed Structures in Chronic Wounds
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Kimberly Brock, RN, WCC; Mckena Cox, RN, BSN; Dana Johnson, RN, WCC; Terri Solomon, RN, WCC, OMS
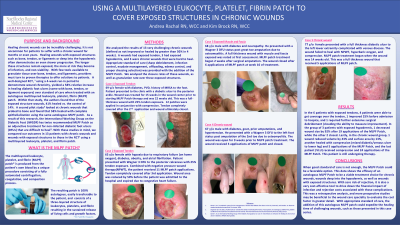
Introduction: Healing chronic diabetic foot ulcers (DFU) can be incredibly challenging, especially those with exposed structures such as bone, tendon, or ligaments or deep into the hypodermis. The longer these structures remain exposed, the more at risk they become of infection and non-viability. With few tools available to granulate tissue over exposed structures, providers must turn to proven therapies such as the multilayered leukocyte, platelet, and fibrin (MLPF) patch. One RCT, ¹ using a 4-week run-in period to demonstrate chronicity, yielded a 58% increase in healing DFUs (some with exposed structures) with the MLPF Patch over standard of care. Within that study, the authors found that of the exposed structure wounds, 41% healed vs. the control of 14%. A second pilot study² looked at chronic wounds that probed to bone and found 58% healed using the MLPF patch. With these studies in mind, we compared our outcomes in patients with chronic wounds and wounds with exposed structures to those in the RCT¹ using the MLPF patch.
Methods: We analyzed the results of 12 challenging wounds. 6 had exposed tendon, 3 exposed hypodermis, and 3 were chronic long-standing wounds. Wounds were treated with appropriate standard of care (sharp debridement, infection control, exudate and edema management, offloading, and proper dressing selection) and the MLPF Patch. We analyzed the granulation and closure rates of these wounds.
Results: In the 6 patients with exposed tendons, 4 achieved coverage over the tendon, 1 improved 25% before admission to hospice, and 1 required further surgical debridement. In the 3 with exposed hypodermis, 1 decreased wound size by 92% after 19 applications of the MLPF Patch, while the other 2 healed. Lastly, in the chronic wound group, 1 wound reduced volume by 43%, another healed with compression (mixed diabetic/venous ulcer) and 5 applications of the MLPF Patch, and the last patient (VLU) received compression and 24 applications of the MLPF Patch. This patient is still undergoing therapy.
Discussion: This data shows the efficacy of an autologous MLPF Patch as a viable treatment for chronic wounds, wounds into the hypodermis, and wounds with exposed structures. With zero risk of rejection, it is also a very cost-effective tool. This was a retrospective analysis, and more prospective studies may be beneficial to evaluate the cost factor in greater detail. With appropriate standard of care, the addition of this autologous MLPF patch could expedite the healing time of challenging wounds.
Methods: We analyzed the results of 12 challenging wounds. 6 had exposed tendon, 3 exposed hypodermis, and 3 were chronic long-standing wounds. Wounds were treated with appropriate standard of care (sharp debridement, infection control, exudate and edema management, offloading, and proper dressing selection) and the MLPF Patch. We analyzed the granulation and closure rates of these wounds.
Results: In the 6 patients with exposed tendons, 4 achieved coverage over the tendon, 1 improved 25% before admission to hospice, and 1 required further surgical debridement. In the 3 with exposed hypodermis, 1 decreased wound size by 92% after 19 applications of the MLPF Patch, while the other 2 healed. Lastly, in the chronic wound group, 1 wound reduced volume by 43%, another healed with compression (mixed diabetic/venous ulcer) and 5 applications of the MLPF Patch, and the last patient (VLU) received compression and 24 applications of the MLPF Patch. This patient is still undergoing therapy.
Discussion: This data shows the efficacy of an autologous MLPF Patch as a viable treatment for chronic wounds, wounds into the hypodermis, and wounds with exposed structures. With zero risk of rejection, it is also a very cost-effective tool. This was a retrospective analysis, and more prospective studies may be beneficial to evaluate the cost factor in greater detail. With appropriate standard of care, the addition of this autologous MLPF patch could expedite the healing time of challenging wounds.

.jpg)