Case Series/Study
(CS-110) Valbenazine Treatment for Tardive Dyskinesia in a 64-year-old Bipolar Female with Chronic Wounds Due to Hypermobility: A Case Report
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Samera Taki, BS – Clinical Research Coordinator, Mobile Doctor Medical Clinic
Introduction: Tardive dyskinesia (TD) is a movement disorder characterized by involuntary movements developing from dopamine receptor-blocking agents, with long term use of first-generation antipsychotics associated with higher risk1. This case evaluates efficacy of valbenazine for a newly-diagnosed TD patient with lumbar ulcers that failed conservative treatment. Patient was a 64-year-old female with hypothyroidism, pancreatitis, osteoporosis, levoscoliosis, GERD, and BD-I; patient had ten years of quetiapine use, with dosage lowered two months before initial presentation. Wounds were not resolved until proper consideration of effect of dyskinesia on wounds and subsequent treatment.
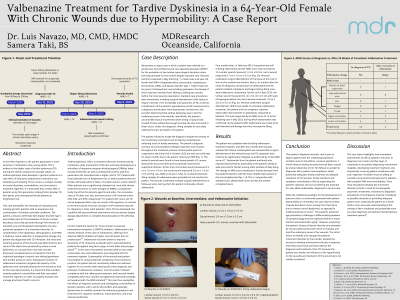
Methods: Patient presented with two lumbar stage-4 decubitus ulcers that had persisted for five months despite standard care and developed osteomyelitis, subsequently resolved with dicloxacillin. At presentation, lumbar wound measured 2.2cm x 1.0cm x 1.0cm, sacral wound 3.0cm x 1.5cm x 0.3cm. Symptoms of a movement disorder suggested TD prognosis, supported by AIMS2 score of 12. Valbenazine was prescribed but not taken for six months due to patient’s diagnosis aversion; serial debridement was performed throughout. At time of valbenazine initiation, lumbar wound measured 0.4cm x 0.4cm x 0.3cm, sacral wound 1.0cm x 2.0cm x 0.5cm, AIMS score was 8. After two weeks, dosage was increased. Within four months, both wounds achieved closure and final AIMS score was 7.
Results: Comprehensive evaluation of patient’s trunkal hyperkinesia in the context of AP history informed a TD diagnosis and subsequent initiation of valbenazine, which enabled wound closures within five months. Overall improvement in TD was reflected by a 5-point decrease in AIMS score. While the traditional paradigm for the development of decubitus ulcers is usually associated with hypomobility or immobility, this case reports lumbar ulcers arising from shear force caused by intense trunkal dyskinesia.
Discussion: This case highlights the importance of holistic patient assessments in diagnosing concomitant maladies, and how patient aversion and noncompliance can further complicate treatment regimens. While decubitus wound paradigms are generally linked to pressure ulcers, this case exemplifies how providers must be willing to consider potentially unorthodox phenomena in order to properly determine and treat comorbid conditions.
Methods: Patient presented with two lumbar stage-4 decubitus ulcers that had persisted for five months despite standard care and developed osteomyelitis, subsequently resolved with dicloxacillin. At presentation, lumbar wound measured 2.2cm x 1.0cm x 1.0cm, sacral wound 3.0cm x 1.5cm x 0.3cm. Symptoms of a movement disorder suggested TD prognosis, supported by AIMS2 score of 12. Valbenazine was prescribed but not taken for six months due to patient’s diagnosis aversion; serial debridement was performed throughout. At time of valbenazine initiation, lumbar wound measured 0.4cm x 0.4cm x 0.3cm, sacral wound 1.0cm x 2.0cm x 0.5cm, AIMS score was 8. After two weeks, dosage was increased. Within four months, both wounds achieved closure and final AIMS score was 7.
Results: Comprehensive evaluation of patient’s trunkal hyperkinesia in the context of AP history informed a TD diagnosis and subsequent initiation of valbenazine, which enabled wound closures within five months. Overall improvement in TD was reflected by a 5-point decrease in AIMS score. While the traditional paradigm for the development of decubitus ulcers is usually associated with hypomobility or immobility, this case reports lumbar ulcers arising from shear force caused by intense trunkal dyskinesia.
Discussion: This case highlights the importance of holistic patient assessments in diagnosing concomitant maladies, and how patient aversion and noncompliance can further complicate treatment regimens. While decubitus wound paradigms are generally linked to pressure ulcers, this case exemplifies how providers must be willing to consider potentially unorthodox phenomena in order to properly determine and treat comorbid conditions.

.jpg)