Case Series/Study
(CS-072) Working in Synergy to Heal: Integrating Multimodal Therapies with Comprehensive Monitoring
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Introduction: Chronic, non-healing wounds pose significant challenges in clinical practice, placing substantial burdens on patients, caregivers, healthcare providers, and payers.¹,² A multimodal therapeutic strategy, enhanced by advanced monitoring technologies, is critical for achieving optimal wound healing outcomes. This work aims to demonstrate the clinical efficacy and cost-effectiveness of integrating multimodal therapeutic strategy with advanced monitoring technologies. Through a comprehensive approach, this case study illustrates how chronic wounds in patients with complex comorbidities can be effectively managed.
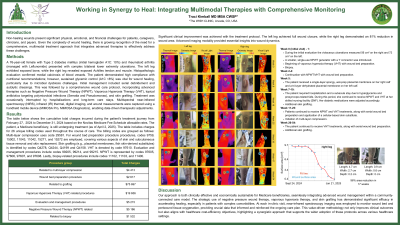
Methods: A 76-year-old female with Type 2 diabetes mellitus (initial hemoglobin A1C: 10%) and rheumatoid arthritis (managed with Leflunomide) presented with complex bilateral lower extremity ulcerations. The left leg exhibited exposed bone, while the right leg revealed exposed Achilles tendon and muscle. Histopathologic evaluation confirmed medial calcinosis of blood vessels. The patient demonstrated high compliance with nutritional recommendations; however, sustained glycemic control (A1C < 8%) was vital for wound healing, particularly due to microbial dysbiosis challenges.
Initial management included serial debridement and autolytic dressings. This was followed by a 15-week comprehensive wound care protocol, incorporating advanced therapies such as Negative Pressure Wound Therapy, Vaporous Hyperoxia Therapy, topical antibiotics targeting polymicrobial infections (Serratia and Pseudomonas), and cellular tissue products (CTPs). Treatment was occasionally interrupted by hospitalizations and long-term care stays.
Monitoring tools, including Near-Infrared Spectroscopy (NIRS), infrared thermography,³,⁴ and wound measurements, assessed tissue oxygenation, skin temperature, and wound dimensions, enabling data-driven therapeutic adjustments.
Results: Significant clinical improvement was achieved with the treatment protocol. The left leg achieved full wound closure, while the right leg demonstrated an 81% reduction in wound area. Advanced imaging modalities provided essential insights into wound dynamics. NIRS revealed progressive tissue oxygenation improvements, and thermography demonstrated normalization of skin temperature, indicative of enhanced perfusion and reduced inflammation.
Moreover, the economic implications of this integrated approach cannot be overstated. Cumulative charges, calculated using the Novitas Medicare Fee Schedule, covered 47 unique billing codes, with all services reimbursed by insurance.
Discussion: This case highlights the clinical efficacy and cost-effectiveness of an integrated multimodal wound care strategy. By combining innovative therapies with robust monitoring tools, this approach successfully addresses chronic wounds in patients with complex comorbidities. It also offers a scalable model for broader implementation, aligning with goals for improved clinical outcomes and healthcare cost efficiency.
Methods: A 76-year-old female with Type 2 diabetes mellitus (initial hemoglobin A1C: 10%) and rheumatoid arthritis (managed with Leflunomide) presented with complex bilateral lower extremity ulcerations. The left leg exhibited exposed bone, while the right leg revealed exposed Achilles tendon and muscle. Histopathologic evaluation confirmed medial calcinosis of blood vessels. The patient demonstrated high compliance with nutritional recommendations; however, sustained glycemic control (A1C < 8%) was vital for wound healing, particularly due to microbial dysbiosis challenges.
Initial management included serial debridement and autolytic dressings. This was followed by a 15-week comprehensive wound care protocol, incorporating advanced therapies such as Negative Pressure Wound Therapy, Vaporous Hyperoxia Therapy, topical antibiotics targeting polymicrobial infections (Serratia and Pseudomonas), and cellular tissue products (CTPs). Treatment was occasionally interrupted by hospitalizations and long-term care stays.
Monitoring tools, including Near-Infrared Spectroscopy (NIRS), infrared thermography,³,⁴ and wound measurements, assessed tissue oxygenation, skin temperature, and wound dimensions, enabling data-driven therapeutic adjustments.
Results: Significant clinical improvement was achieved with the treatment protocol. The left leg achieved full wound closure, while the right leg demonstrated an 81% reduction in wound area. Advanced imaging modalities provided essential insights into wound dynamics. NIRS revealed progressive tissue oxygenation improvements, and thermography demonstrated normalization of skin temperature, indicative of enhanced perfusion and reduced inflammation.
Moreover, the economic implications of this integrated approach cannot be overstated. Cumulative charges, calculated using the Novitas Medicare Fee Schedule, covered 47 unique billing codes, with all services reimbursed by insurance.
Discussion: This case highlights the clinical efficacy and cost-effectiveness of an integrated multimodal wound care strategy. By combining innovative therapies with robust monitoring tools, this approach successfully addresses chronic wounds in patients with complex comorbidities. It also offers a scalable model for broader implementation, aligning with goals for improved clinical outcomes and healthcare cost efficiency.

.jpg)