Case Series/Study
(CS-167) Treating Chronic Pyoderma Gangrenosum with Vaporous Hyperoxia Therapy: A Case Report
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Introduction: Pyoderma gangrenosum (PG) is a rare, chronic inflammatory skin condition characterized by painful, non-healing ulcers. Standard management often includes systemic immunosuppressants and topical therapies; however, many cases remain refractory to treatment. This study highlights the successful resolution of chronic PG in a 62-year-old female using Vaporous Hyperoxia Therapy (VHT®) as an adjunct to standard care.
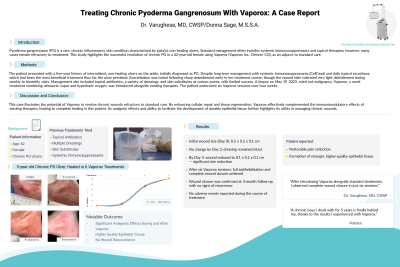
Methods: The patient presented with a five-year history of intermittent, non-healing ulcers on the ankle, initially diagnosed as PG. Despite long-term management with systemic immunosuppressants (CellCept) and daily topical tacrolimus, which had been the most beneficial treatment thus far, the ulcer persisted. Exacerbation was noted following sharp debridement early in her treatment course, though the wound later tolerated very light debridement during weekly to biweekly visits. Management also included topical antibiotics, a variety of dressings, and skin substitutes at various points, with limited success. A biopsy on May 19, 2023, ruled out malignancy. VHT®, a novel treatment combining ultrasonic vapor and hyperbaric oxygen, was introduced alongside existing therapies. The patient underwent six VHT® sessions over four weeks.
Results: At the start of VHT® (Day 0), the wound measured 0.2 x 0.2 x 0.1 cm. The wound dressing remained intact at Day 3, with measurements unchanged. By Day 5, the wound had decreased in size to 0.1 x 0.1 x 0.1 cm, reflecting significant progress over just five days. Following six VHT® sessions, full epithelialization and complete wound closure were achieved, with significant analgesic effects. As the wound healed, the patient reported decreased pain and soreness, as well as the development of higher-quality epithelial tissue likely to withstand future breakdown. The wound has remained resolved for three months. No adverse events were reported during the treatment period.
Discussion: This case illustrates the potential of VHT® to resolve chronic wounds refractory to standard care. By enhancing cellular repair and tissue regeneration, VHT® effectively complemented the immunomodulatory effects of existing therapies, leading to complete healing in this patient. Its analgesic effects and ability to facilitate the development of durable epithelial tissue further highlights its utility in managing chronic wounds.
Conclusion:
VHT® successfully resolved a chronic PG wound that had been resistant to conventional therapies, underscoring its value as an advanced wound care modality. Further research is warranted to explore the broader clinical applications of VHT® in managing complex and chronic wounds.
Methods: The patient presented with a five-year history of intermittent, non-healing ulcers on the ankle, initially diagnosed as PG. Despite long-term management with systemic immunosuppressants (CellCept) and daily topical tacrolimus, which had been the most beneficial treatment thus far, the ulcer persisted. Exacerbation was noted following sharp debridement early in her treatment course, though the wound later tolerated very light debridement during weekly to biweekly visits. Management also included topical antibiotics, a variety of dressings, and skin substitutes at various points, with limited success. A biopsy on May 19, 2023, ruled out malignancy. VHT®, a novel treatment combining ultrasonic vapor and hyperbaric oxygen, was introduced alongside existing therapies. The patient underwent six VHT® sessions over four weeks.
Results: At the start of VHT® (Day 0), the wound measured 0.2 x 0.2 x 0.1 cm. The wound dressing remained intact at Day 3, with measurements unchanged. By Day 5, the wound had decreased in size to 0.1 x 0.1 x 0.1 cm, reflecting significant progress over just five days. Following six VHT® sessions, full epithelialization and complete wound closure were achieved, with significant analgesic effects. As the wound healed, the patient reported decreased pain and soreness, as well as the development of higher-quality epithelial tissue likely to withstand future breakdown. The wound has remained resolved for three months. No adverse events were reported during the treatment period.
Discussion: This case illustrates the potential of VHT® to resolve chronic wounds refractory to standard care. By enhancing cellular repair and tissue regeneration, VHT® effectively complemented the immunomodulatory effects of existing therapies, leading to complete healing in this patient. Its analgesic effects and ability to facilitate the development of durable epithelial tissue further highlights its utility in managing chronic wounds.
Conclusion:
VHT® successfully resolved a chronic PG wound that had been resistant to conventional therapies, underscoring its value as an advanced wound care modality. Further research is warranted to explore the broader clinical applications of VHT® in managing complex and chronic wounds.

.jpg)