Case Series/Study
(CS-025) Pyoderma Gangrenosum: A Comprehensive Analysis of Comorbidities and Prognosis
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Alessandra Michelucci, MD; Giammarco Granieri, MD; Irina Balan, MD; Valentina Dini, PhD; Marco Romanelli, PhD
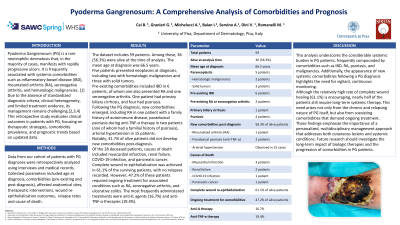
Introduction: Pyoderma Gangrenosum (PG) is a rare neutrophilic dermatosis causing rapidly progressive ulcers. It is often associated with systemic conditions like inflammatory bowel disease (IBD), rheumatoid arthritis (RA), and hematologic malignancies. Clinical management is challenging due to diagnostic heterogeneity and limited treatment evidence. This retrospective study evaluates outcomes in 59 PG patients, focusing on comorbidities, therapeutic approaches, and prognostic trends.
Methods: Data from 59 patients with confirmed PG diagnoses since 2013 were retrospectively analysed via interviews and medical records. Key parameters included age at diagnosis, comorbidities, anatomical sites affected, therapies, wound healing, and relapse rates.
Results: Among the 59 patients (41 female and 12 male), 32 (54%) were alive at the time of analysis; the results focus on this subgroup. The mean age at diagnosis was 68.8 years. Five patients presented with neoplasms (two hematologic malignancies and three solid tumours) at diagnosis. Pre-existing comorbidities included IBD (4 cases), RA and ankylosing spondylitis (AS; 1 case), primary biliary cirrhosis (1 case), and psoriasis (2 cases, 1 paraneoplastic). New comorbidities post-diagnosis included RA (1 case), paradoxical psoriasis during anti-TNF-α therapy (2 cases), arterial hypertension, osteoporosis, and myocardial infarction. Notably, 40.6% of alive patients developed no new comorbidities. Complete wound re-epithelialization occurred in 62.5% of survivors, with no reported relapses. However, 45% required ongoing therapy for associated conditions (e.g., RA, AS, ulcerative colitis). Two patients underwent amputation of the affected leg. Anti-IL and anti-TNF-α therapies were the most used treatments, in 15.62% and 18.75% of cases, respectively.
Discussion: This study highlights the significant systemic burden of PG, with frequent pre-existing conditions like IBD, RA, and psoriasis. The emergence of new comorbidities post-diagnosis underscores the disease's dynamic nature. The absence of new conditions in 40.6% of survivors suggests variability in systemic progression. The high rate of wound healing (62.5%) is promising, though ongoing therapy requirements in 45% reflect PG's chronicity. These findings emphasize the need for individualized, multidisciplinary management to address skin and systemic involvement. Future research should focus on the temporal evolution of comorbidities and long-term biologic therapy outcomes.
Methods: Data from 59 patients with confirmed PG diagnoses since 2013 were retrospectively analysed via interviews and medical records. Key parameters included age at diagnosis, comorbidities, anatomical sites affected, therapies, wound healing, and relapse rates.
Results: Among the 59 patients (41 female and 12 male), 32 (54%) were alive at the time of analysis; the results focus on this subgroup. The mean age at diagnosis was 68.8 years. Five patients presented with neoplasms (two hematologic malignancies and three solid tumours) at diagnosis. Pre-existing comorbidities included IBD (4 cases), RA and ankylosing spondylitis (AS; 1 case), primary biliary cirrhosis (1 case), and psoriasis (2 cases, 1 paraneoplastic). New comorbidities post-diagnosis included RA (1 case), paradoxical psoriasis during anti-TNF-α therapy (2 cases), arterial hypertension, osteoporosis, and myocardial infarction. Notably, 40.6% of alive patients developed no new comorbidities. Complete wound re-epithelialization occurred in 62.5% of survivors, with no reported relapses. However, 45% required ongoing therapy for associated conditions (e.g., RA, AS, ulcerative colitis). Two patients underwent amputation of the affected leg. Anti-IL and anti-TNF-α therapies were the most used treatments, in 15.62% and 18.75% of cases, respectively.
Discussion: This study highlights the significant systemic burden of PG, with frequent pre-existing conditions like IBD, RA, and psoriasis. The emergence of new comorbidities post-diagnosis underscores the disease's dynamic nature. The absence of new conditions in 40.6% of survivors suggests variability in systemic progression. The high rate of wound healing (62.5%) is promising, though ongoing therapy requirements in 45% reflect PG's chronicity. These findings emphasize the need for individualized, multidisciplinary management to address skin and systemic involvement. Future research should focus on the temporal evolution of comorbidities and long-term biologic therapy outcomes.

.jpg)