Clinical Research
(CR-025) Real-world Use of Porcine Placental Extracellular Matrix (PPECM)* in Hard-to-heal Wounds
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Ben LeBoutillier, Data Operations Manager – Data Operations Manager, Intellicure; Cristin Taylor, PA – Senior Director Medical Affairs, Convatec; Brad Marcinek, PA – Medical Affairs Manager, Convatec
Introduction: Real-world data are a highly valuable resource in determining the efficacy of novel products in challenging populations, especially in wound care. This analysis of real-world data aims to describe the clinical performance of PPECM*, a novel Cellular, Acellular, Matrix-like Product, in a medically complex patient population with severe, limb-/life-threatening (L/LT) wounds.
Methods: The US Wound Registry (USWR) aggregates highly structured electronic health records (EHRs) from 502 wound centers. From this, a deidentified dataset from 10-Oct.-2022 to 25-Mar.-2024 containing 76,278 patients with 248,278 wounds was screened for patients receiving at least one PPECM* application.
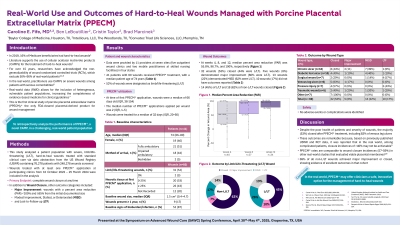
Results: 60 wounds in 41 patients were managed with PPECM*. Median patient age was 74 years [IQR, 66.0 – 80.0], 32 patients (78%) were >65 years old, 49% had impaired ambulation, 12% autoimmune disease, and 12% peripheral arterial disease. Wound types included: chronic ulcers (30%), diabetic ulcers (20%), pressure injuries (12%), dehisced surgical wounds (12%), venous leg ulcers (10%), traumatic wounds (8%), and arterial ulcers (3%). Median wound area was 1.50 cm2 [IQR, 0.42 – 4.69]; most wounds were superficial (n=51), but some exposed deeper tissues including muscle (n=4), tendon (n=2), and bone (n=1). 17% were present >1 year; 87% showed signs of bioburden; and 52% were L/LT. Only 3% had no necrotic tissue at first application and 43% had ≥25%. Wound age at first application of PPECM*, time since first documentation by the practitioner, was 66 days [38.0 – 154.0]. Median PPECM* applications per wound was 2.0 [1.0 – 5.0]. Of 157 total applications, 107 (68%) of selected product sizes were adequate relative to measured wound size. Median percent area reduction at 4-, 8-, and 12-weeks was 50.0% [9.1-97.0, n=43], 88.0% [39.3-100, n=39], and 100% [73.6-100, n=35]. Closure was achieved in 32 wounds (of which 44% were L/LT); 5 showed major improvement (60% L/LT); 13 experienced Modest Improvement, Stalled, or Deteriorated (MISD); 10 did not have outcomes reported. No adverse events or complications were reported.
Discussion: In this real-world dataset, hard-to-heal wounds managed with PPECM showed clinically meaningful, rapid progress toward closure, in the setting of high wound complexity and judicious product utilization.
Methods: The US Wound Registry (USWR) aggregates highly structured electronic health records (EHRs) from 502 wound centers. From this, a deidentified dataset from 10-Oct.-2022 to 25-Mar.-2024 containing 76,278 patients with 248,278 wounds was screened for patients receiving at least one PPECM* application.
Results: 60 wounds in 41 patients were managed with PPECM*. Median patient age was 74 years [IQR, 66.0 – 80.0], 32 patients (78%) were >65 years old, 49% had impaired ambulation, 12% autoimmune disease, and 12% peripheral arterial disease. Wound types included: chronic ulcers (30%), diabetic ulcers (20%), pressure injuries (12%), dehisced surgical wounds (12%), venous leg ulcers (10%), traumatic wounds (8%), and arterial ulcers (3%). Median wound area was 1.50 cm2 [IQR, 0.42 – 4.69]; most wounds were superficial (n=51), but some exposed deeper tissues including muscle (n=4), tendon (n=2), and bone (n=1). 17% were present >1 year; 87% showed signs of bioburden; and 52% were L/LT. Only 3% had no necrotic tissue at first application and 43% had ≥25%. Wound age at first application of PPECM*, time since first documentation by the practitioner, was 66 days [38.0 – 154.0]. Median PPECM* applications per wound was 2.0 [1.0 – 5.0]. Of 157 total applications, 107 (68%) of selected product sizes were adequate relative to measured wound size. Median percent area reduction at 4-, 8-, and 12-weeks was 50.0% [9.1-97.0, n=43], 88.0% [39.3-100, n=39], and 100% [73.6-100, n=35]. Closure was achieved in 32 wounds (of which 44% were L/LT); 5 showed major improvement (60% L/LT); 13 experienced Modest Improvement, Stalled, or Deteriorated (MISD); 10 did not have outcomes reported. No adverse events or complications were reported.
Discussion: In this real-world dataset, hard-to-heal wounds managed with PPECM showed clinically meaningful, rapid progress toward closure, in the setting of high wound complexity and judicious product utilization.

.jpg)