Clinical Research
(CR-027) Retrospective Analysis of Understudied Real-world Complicated and Persistent Diabetic Foot Ulcers: Use of Retention-processed Placental Membranes vs SOC
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Zwelithini Tunyiswa, B.A. – Chief Executive Officer, Open Wound Research; Toni-Ann Martorano, M.S. – Research Associate, R&D, Biostem Technologies; Wendy Weston, PhD, CTBS – VP Research & Development, R&D, Biostem Technologies
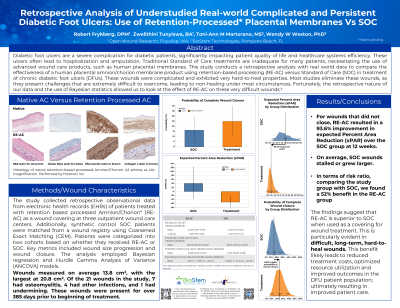
Introduction: Diabetic foot ulcers are a severe complication for diabetic patients, significantly impacting patient quality of life and healthcare systems efficiency. These ulcers often lead to hospitalization and amputation. Traditional Standard of Care treatments are inadequate for many patients, necessitating the use of advanced wound care products, such as human placental membranes. This study conducts a retrospective analysis with real world data to compare the effectiveness of a human placental amnion/chorion membrane product using retention-based processing (RE-AC) versus Standard of Care (SOC) in treatment of chronic diabetic foot ulcers (DFUs). These wounds were complicated and exhibited very hard-to-heal properties. Most studies eliminate these wounds, as they present challenges that are extremely difficult to overcome, leading to non-healing under most circumstances. Fortunately, the retrospective nature of our data and the use of Bayesian statistics allowed us to look at the effect of RE-AC on these very difficult wounds.
Methods: The study collected retrospective observational data from electronic health records (EHRs) of patients treated with retention based processed Amnion/Chorion* (RE-AC) as a wound covering at three outpatient wound care centers. Additionally, synthetic control SOC patients were matched from a wound registry using Coarsened Exact Matching (CEM). Patients were categorized into two cohorts based on whether they received RE-AC or SOC. Key metrics included wound size progression and wound closure. The analysis employed Bayesian regression and Hurdle Gamma Analysis of Variance (ANCOVA) models. Wounds measured on average 13.8 cm2, with the largest at 20.8 cm2. Of the 21 wounds in the study, 7 had osteomyelitis, 4 had other infections, and 1 had undermining. These wounds were present for over 385 days prior to beginning of treatment.
Results: Results indicated that RE-AC achieved approximately 10% higher expected wound closure rate compared to SOC at 12 weeks. Further, for wounds that did not close, RE-AC resulted in approximately 60% expected Percent Area Reduction (xPAR), whereas SOC wounds stalled or grew larger.
Discussion: The findings suggest that RE-AC is superior to SOC when used as a covering for wound treatment This benefit likely leads to reduced treatment costs, optimized resource utilization and improved outcomes in the DFU patient population; ultimately resulting in improved patient care.
Methods: The study collected retrospective observational data from electronic health records (EHRs) of patients treated with retention based processed Amnion/Chorion* (RE-AC) as a wound covering at three outpatient wound care centers. Additionally, synthetic control SOC patients were matched from a wound registry using Coarsened Exact Matching (CEM). Patients were categorized into two cohorts based on whether they received RE-AC or SOC. Key metrics included wound size progression and wound closure. The analysis employed Bayesian regression and Hurdle Gamma Analysis of Variance (ANCOVA) models. Wounds measured on average 13.8 cm2, with the largest at 20.8 cm2. Of the 21 wounds in the study, 7 had osteomyelitis, 4 had other infections, and 1 had undermining. These wounds were present for over 385 days prior to beginning of treatment.
Results: Results indicated that RE-AC achieved approximately 10% higher expected wound closure rate compared to SOC at 12 weeks. Further, for wounds that did not close, RE-AC resulted in approximately 60% expected Percent Area Reduction (xPAR), whereas SOC wounds stalled or grew larger.
Discussion: The findings suggest that RE-AC is superior to SOC when used as a covering for wound treatment This benefit likely leads to reduced treatment costs, optimized resource utilization and improved outcomes in the DFU patient population; ultimately resulting in improved patient care.

.jpg)