Case Series/Study
(CS-013) Saving the Foot: A Novel Approach to Vasopressor-induced Ischemia
Vasopressors are essential for managing critically ill patients in septic shock to maintain blood pressure. However, a serious complication is vasopressor-induced digital ischemia, resulting from decreased digital perfusion. These ischemic changes are often irreversible, frequently leading to amputations. When soft tissue necrosis extends proximally beyond the amputation margins, surgical closure becomes challenging.
To address such challenges, skin graft substitutes can be employed to promote closure and dermal augmentation. Acellular fish skin grafts, in particular, provide an optimal scaffold for human fibroblast incorporation, enabling rapid integration. Additionally, fish skin grafts offer antimicrobial, anti-inflammatory, and analgesic properties, which are particularly beneficial in immunocompromised patients.
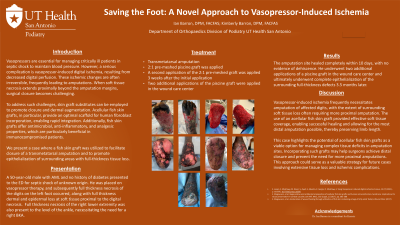
We present a case where a fish skin graft was utilized to facilitate closure of a transmetatarsal amputation and to promote epithelialization of surrounding areas with full-thickness tissue loss.
Methods: This case involves a patient who underwent a transmetatarsal amputation due to vasopressor-induced ischemia, with minimal viable soft tissue available for closure. A pre-meshed (2:1) fish skin graft was applied directly to the incision and adjacent full-thickness tissue defects after the initial amputation. Ten days later, the site underwent a second debridement, followed by reapplication of the pre-meshed fish skin graft.
Results: The amputation site healed completely within 10 days, with no evidence of dehiscence. Epithelialization of the surrounding full-thickness defects progressed steadily, resulting in complete healing of the amputation site.
Discussion:
Vasopressor-induced ischemia frequently necessitates amputation of affected digits, with the extent of surrounding soft tissue loss often requiring more proximal amputation. The use of an acellular fish skin graft provided effective soft tissue coverage, enabling successful healing and allowing for the most distal amputation possible, thereby preserving limb length.
This case highlights the potential of acellular fish skin grafts as a viable option for managing complex tissue deficits in amputation sites. Incorporating such grafts may help surgeons achieve distal closure and prevent the need for more proximal amputations. This approach could serve as a valuable strategy for future cases involving extensive tissue loss and ischemic complications.

.jpg)