Clinical Research
(CR-069 (RPT-001)) Pediatric Chronic Wounds: A Novel Analysis from a Tertiary Care Center
Friday, May 2, 2025
4:45 PM - 5:45 PM East Coast USA Time
Catherine Kennedy, BHSc; Michael Nieveras, BS; Kaylee Leathers, MD; Josh Bricker, PhD; Jenny Barker, MD, PhD
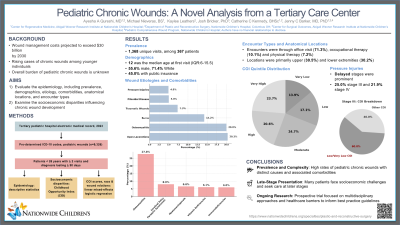
Introduction: 10.5 million Americans suffer from chronic wounds annually. While extensively studied in adults, pediatric chronic wounds receive limited attention, relying on adult-centric approaches and anecdotal evidence. Our study is among the first to (1) describe the prevalence and demographics of pediatric chronic wounds, (2) evaluate wound presentations including etiologies, comorbidities, anatomical locations, and encounter types; and (3) examine the socioeconomic disparities influencing their development.
Methods: We conducted a retrospective analysis of visits for wounds at a tertiary pediatric hospital in 2023, based on a coding schema including 9,326 pre-determined ICD-10 codes. Patients under age 26 with >2 visits and diagnosed chronic wounds lasting >90 days were included. Socioeconomic disparities were evaluated using the Childhood Opportunity Index (COI). Linear mixed-effects logistic regression models examined the relationships between COI scores, race and wound characteristics.
Results: We identified 1,368 unique visits among 367 chronic wound patients. Median age at first visit was 12(IQR:6–15.5), 55.6% were male, 71.4% White, and 45.0% had public insurance. Most prevalent wounds included open lacerations (20.3%), osteomyelitis (20.0%), burns (14.2%), traumatic (7.3%), pilonidal (5.0%), and pressure injuries (4.9%). Comorbidities were notable for osteomyelitis (27.8%), cerebral palsy/paralytic syndromes (8.0%), myelomeningocele (6.6%), vitamin deficiencies (6.1%), and immunodeficiencies (6.0%). Anatomical locations were primarily upper (30.5%) and lower extremities (30.2%). Encounters were primarily through office visit (71.3%), occupational therapy (10.1%) and physical therapy (7.2%).
COI quintile distribution was very low (13.9%), low (17.1%), moderate (24.7%), high (20.6%), and very high (23.7%). Regression demonstrated COI scores were not associated with wound development and race was not associated with wound severity. Of those who had pressure injuries, stage III (25.0%) and IV (21.9%) were most common. 60% of stage III cases had a low or very low COI, suggesting potential disparities which may affect timely interventions.
Discussion: Building on our prior national analysis, this study highlights a high prevalence of pediatric chronic wounds with distinct etiologies and comorbidities. Many of these patients face socioeconomic challenges and present at late stages. Our ongoing research thus includes a prospective trial investigating multidisciplinary wound presentations and healthcare barriers to develop best practice guidelines for this vulnerable group.
Methods: We conducted a retrospective analysis of visits for wounds at a tertiary pediatric hospital in 2023, based on a coding schema including 9,326 pre-determined ICD-10 codes. Patients under age 26 with >2 visits and diagnosed chronic wounds lasting >90 days were included. Socioeconomic disparities were evaluated using the Childhood Opportunity Index (COI). Linear mixed-effects logistic regression models examined the relationships between COI scores, race and wound characteristics.
Results: We identified 1,368 unique visits among 367 chronic wound patients. Median age at first visit was 12(IQR:6–15.5), 55.6% were male, 71.4% White, and 45.0% had public insurance. Most prevalent wounds included open lacerations (20.3%), osteomyelitis (20.0%), burns (14.2%), traumatic (7.3%), pilonidal (5.0%), and pressure injuries (4.9%). Comorbidities were notable for osteomyelitis (27.8%), cerebral palsy/paralytic syndromes (8.0%), myelomeningocele (6.6%), vitamin deficiencies (6.1%), and immunodeficiencies (6.0%). Anatomical locations were primarily upper (30.5%) and lower extremities (30.2%). Encounters were primarily through office visit (71.3%), occupational therapy (10.1%) and physical therapy (7.2%).
COI quintile distribution was very low (13.9%), low (17.1%), moderate (24.7%), high (20.6%), and very high (23.7%). Regression demonstrated COI scores were not associated with wound development and race was not associated with wound severity. Of those who had pressure injuries, stage III (25.0%) and IV (21.9%) were most common. 60% of stage III cases had a low or very low COI, suggesting potential disparities which may affect timely interventions.
Discussion: Building on our prior national analysis, this study highlights a high prevalence of pediatric chronic wounds with distinct etiologies and comorbidities. Many of these patients face socioeconomic challenges and present at late stages. Our ongoing research thus includes a prospective trial investigating multidisciplinary wound presentations and healthcare barriers to develop best practice guidelines for this vulnerable group.

.jpg)
