Case Series/Study
(CS-137) Peptide-based Biomimetic Matrix Achieves Rapid Closure of Chronic Venous Leg Ulcers
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Introduction: Venous Leg Ulcers (VLUs) are challenging wounds associated with healthcare costs estimated at >$32 billion annually1, given the delayed healing and high recurrence rates, with only 60% closing by 12 weeks and 75% reappearing within 3 weeks2. Despite the severity of the issue and the recent advancements in wound care, VLUs remain an unmet clinical need requiring novel approaches. The objective of this study was to evaluate the safety and performance of an innovative Biomimetic Matrix (BMM) in chronic VLU management. Designed to promote tissue regrowth and prevent infection, BMM is a synthetic extracellular matrix (ECM)-like scaffold made of antibacterial self-assembling peptides that completely conforms to irregular, deep, and hard-to-access wounds.
Methods: Patients with multiple comorbidities [including peripheral vascular disease, diabetes, rheumatoid arthritis, limited mobility, lymphedema] presenting chronic VLUs were selected to receive an FDA-approved peptide-based BMM*. BMM was used after proper wound bed preparation per the manufacturer’s instructions. Wound size measurements were captured at baseline and at each following visit using an artificial intelligence (AI) based imaging software. Clinical observations were recorded at each visit, including wound and peri-wound skin appearance.
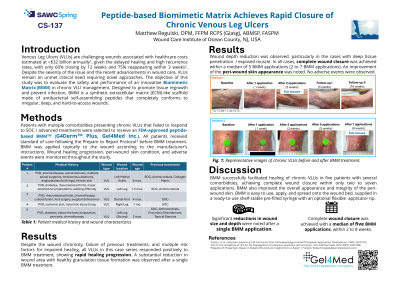
Results: All VLUs in this case series responded positively to BMM treatment, showing fast healing progression. Complete wound closure was achieved within the study period in all five ulcers. In two cases, approximately 50% surface area reduction was observed after a single application with full wound closure achieved within five applications of BMM. In three other cases, while the first application did not result in such a marked surface wound area reduction (percent area reduction ranging between 7% and 38%), full closure was still achieved within three to five BMM applications. A substantial decrease in wound depth was also observed. In all five cases, early formation of healthy granulation tissue and an improvement in peri-wound skin appearance were noted with BMM treatment. No adverse events were observed.
Discussion: This small case series establishes the potential of BMM in treating chronic VLUs by promoting early granulation tissue formation and rapid wound closure. Future studies in a larger population are needed to validate and expand these findings.
Methods: Patients with multiple comorbidities [including peripheral vascular disease, diabetes, rheumatoid arthritis, limited mobility, lymphedema] presenting chronic VLUs were selected to receive an FDA-approved peptide-based BMM*. BMM was used after proper wound bed preparation per the manufacturer’s instructions. Wound size measurements were captured at baseline and at each following visit using an artificial intelligence (AI) based imaging software. Clinical observations were recorded at each visit, including wound and peri-wound skin appearance.
Results: All VLUs in this case series responded positively to BMM treatment, showing fast healing progression. Complete wound closure was achieved within the study period in all five ulcers. In two cases, approximately 50% surface area reduction was observed after a single application with full wound closure achieved within five applications of BMM. In three other cases, while the first application did not result in such a marked surface wound area reduction (percent area reduction ranging between 7% and 38%), full closure was still achieved within three to five BMM applications. A substantial decrease in wound depth was also observed. In all five cases, early formation of healthy granulation tissue and an improvement in peri-wound skin appearance were noted with BMM treatment. No adverse events were observed.
Discussion: This small case series establishes the potential of BMM in treating chronic VLUs by promoting early granulation tissue formation and rapid wound closure. Future studies in a larger population are needed to validate and expand these findings.

.jpg)