Laboratory Research
(LR-012) In vitro Assessment of a Methylene Blue and Gentian Violet-containing Foam Dressing and an Advanced Silver-containing Gelling Fiber Dressing Against Surface-associated Antibiotic-resistant Bacteria
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Kate Meredith, PhD – Principal Scientist, Microbiology, Convatec; Daniel Metcalf, PhD – Director, Advanced Wound Care R&D, Convatec Ltd
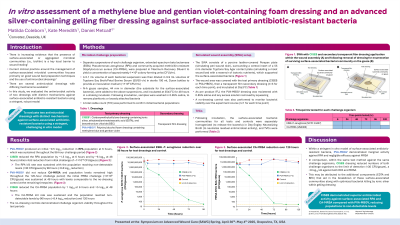
Introduction: Microorganisms in surface-associated/aggregated form are implicated in hard-to-heal wounds and comprise communities embedded in extracellular polymeric substance (EPS) matrices. In vitro studies have assessed the antimicrobial efficacy of wound dressings against this phenotype; however, methods vary in robustness and validity. We evaluated two antimicrobial dressings with distinct mechanisms against antibiotic-resistant bacteria using a stringent, challenging in vitro model.
Methods: A carboxymethylcellulose fiber dressing* containing ionic silver, ethylenediaminetetraacetic acid (EDTA) and benzethonium chloride (BEC; ‘CISEB’) and a polyvinyl alcohol foam dressing† containing methylene blue and gentian violet (‘PVA-MBGV’) were evaluated. Challenge bacteria (antibiotic-resistant Pseudomonas aeruginosa [RPA] and community-associated methicillin-resistant Staphylococcus aureus [CA-MRSA]) were separately grown on gauze (simulating surface-associated/aggregated phenotype) and transferred to simulated wound assemblies. Test dressings were applied to the colonized gauzes and covered with a transparent film dressing before incubation for ≤120 hours at 35±3ºC. A no-dressing control was included. Enumeration of surviving bacteria was performed for each test dressing (n=3).
Results: PVA-MBGV produced an initial ~0.5 log10 reduction in RPA population at 6 hours, which was sustained throughout the 96-hour challenge period. CISEB reduced the RPA population by ~1.5 log10 at 6 hours and by ~6 log10 at 48 hours (million-fold reduction from initial challenge of ~1×1010 colony-forming units [CFU]/gauze). The kill rate was sustained with the population reaching non-detectable levels (< 30 CFU/gauze) by 96 hours (~8.8 log10 reduction). No reduction in CA-MRSA was observed with PVA-MBGV and population levels remained high throughout the 120-hour challenge period. The initial bacterial challenge (~3×109 CFU/gauze) was sustained at 48 hours with levels comparable to the no-dressing control at the remaining timepoints. CISEB reduced the CA-MRSA population by 1 log10 at 6 hours and >5 log10 at 48 hours. The kill rate was sustained and the population reached non-detectable levels by 96 hours (~8.4 log10 reduction) and 120 hours. The no-dressing controls demonstrated challenge organism viability throughout the test periods.
Discussion:
CISEB demonstrated superior antimicrobial activity against surface-associated RPA and CA-MRSA compared with PVA-MBGV, reducing populations to non-detectable levels. The observed activity of CISEB may be attributed to EDTA and BEC that can disrupt EPS matrices, potentiating the antimicrobial activity of ionic silver.
Methods: A carboxymethylcellulose fiber dressing* containing ionic silver, ethylenediaminetetraacetic acid (EDTA) and benzethonium chloride (BEC; ‘CISEB’) and a polyvinyl alcohol foam dressing† containing methylene blue and gentian violet (‘PVA-MBGV’) were evaluated. Challenge bacteria (antibiotic-resistant Pseudomonas aeruginosa [RPA] and community-associated methicillin-resistant Staphylococcus aureus [CA-MRSA]) were separately grown on gauze (simulating surface-associated/aggregated phenotype) and transferred to simulated wound assemblies. Test dressings were applied to the colonized gauzes and covered with a transparent film dressing before incubation for ≤120 hours at 35±3ºC. A no-dressing control was included. Enumeration of surviving bacteria was performed for each test dressing (n=3).
Results: PVA-MBGV produced an initial ~0.5 log10 reduction in RPA population at 6 hours, which was sustained throughout the 96-hour challenge period. CISEB reduced the RPA population by ~1.5 log10 at 6 hours and by ~6 log10 at 48 hours (million-fold reduction from initial challenge of ~1×1010 colony-forming units [CFU]/gauze). The kill rate was sustained with the population reaching non-detectable levels (< 30 CFU/gauze) by 96 hours (~8.8 log10 reduction). No reduction in CA-MRSA was observed with PVA-MBGV and population levels remained high throughout the 120-hour challenge period. The initial bacterial challenge (~3×109 CFU/gauze) was sustained at 48 hours with levels comparable to the no-dressing control at the remaining timepoints. CISEB reduced the CA-MRSA population by 1 log10 at 6 hours and >5 log10 at 48 hours. The kill rate was sustained and the population reached non-detectable levels by 96 hours (~8.4 log10 reduction) and 120 hours. The no-dressing controls demonstrated challenge organism viability throughout the test periods.
Discussion:
CISEB demonstrated superior antimicrobial activity against surface-associated RPA and CA-MRSA compared with PVA-MBGV, reducing populations to non-detectable levels. The observed activity of CISEB may be attributed to EDTA and BEC that can disrupt EPS matrices, potentiating the antimicrobial activity of ionic silver.

.jpg)