Laboratory Research
(LR-018) In Vitro Efficacy of a New Formulation Combining Topical Exosome-loaded Gel with Antibiotic Against Gram Positive and Negative Bacteria
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Michael Solis, MBA – Sr. Research Associate 1, Dermatology, University of Miami, Miller School of Medicine. Dr. Phillip Frost Department of Dermatology and Cutaneous Surgery; Ryan Strong, BS – Sr. Research Associate 1, Dermatology, University of Miami, Miller School of Medicine. Dr. Phillip Frost Department of Dermatology and Cutaneous Surgery; Roger Cassagnol, BS – Research Assistant, Dermatology, University of Miami, Miller School of Medicine. Dr. Phillip Frost Department of Dermatology and Cutaneous Surgery; Melissa Wright, PhD – Luna Labs USA; Kate Johnson, PhD – Luna Labs USA; Stephen Davis, BS – Research Professor, Dermatology, University of Miami Miller School of Medicine
Introduction: Bacterial resistance to antibiotics is an important problem, especially in non-healing wounds. Two of the most commons pathogens associated with these infections are Staphylococcus aureus and Acinetobacter baumannii. Exosomes are lipid bilayer-delimited particles that are naturally released from almost all types of cells but, unlike a cell, cannot replicate. They serve as a fundamental intercellular communication system and have shown efficacy in tissue repair. In this in vitro study, we examined the use of antibiotic-loaded exosomes formulated with synthetic liposomes to treat and prevent wound infections.
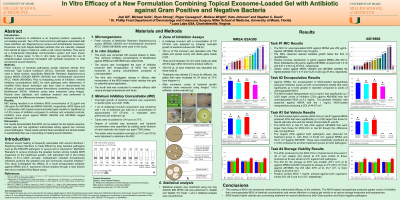
Methods: Fresh cultures of bacterial pathogenic isolate obtained directly from American Type Culture Collection (ATCC), Rockville, Maryland, were used in these studies, specifically Methicillin Resistant Staphylococcus aureus MRSA USA300 (MRSA USA300) and Acinetobacter baumannii ATCC 19606 (AB19606). Prior to evaluating zones of inhibition, minimal inhibitory concentrations (MIC) for each pathogen were determined. A modified Kirby Bauer technique was then used to demonstrate the efficacy of topical exosome-loaded gels containing the antibiotic Moxifloxacin (MOX). Inhibition zones were measured using ImageJ. Results were tabulated, and statistical analysis was performed to demonstrate the differences between treatments.
Results: MIC testing resulted in an inhibitory MOX concentration of 32 mg/ml and 256 mg/ml for AB19606 and MRSA USA300, respectively. MOX alone and in combination with topical exosome-loaded gels resulted in significant (p ≤ 0.05) zones of inhibition compared to vehicles and untreated controls. Inhibition zone areas against MRSA USA300 and AB19606 ranged between 30-43 cm2.
Discussion: Our results demonstrated that MOX can be loaded into the topical exosome-loaded gels and has significant antimicrobial activity against two common wound pathogens. These results warrant future preclinical and clinical studies to substantiate their use in preventing or treating wound infections.
Acknowledgements: This work was supported by US Army Medical Research and Development Command Contract HT9425-24-P-0035. The views, opinions, and findings are those of the author(s) and should not be construed as official Army or DHA position, policy or decision unless designated by other documentation.
Methods: Fresh cultures of bacterial pathogenic isolate obtained directly from American Type Culture Collection (ATCC), Rockville, Maryland, were used in these studies, specifically Methicillin Resistant Staphylococcus aureus MRSA USA300 (MRSA USA300) and Acinetobacter baumannii ATCC 19606 (AB19606). Prior to evaluating zones of inhibition, minimal inhibitory concentrations (MIC) for each pathogen were determined. A modified Kirby Bauer technique was then used to demonstrate the efficacy of topical exosome-loaded gels containing the antibiotic Moxifloxacin (MOX). Inhibition zones were measured using ImageJ. Results were tabulated, and statistical analysis was performed to demonstrate the differences between treatments.
Results: MIC testing resulted in an inhibitory MOX concentration of 32 mg/ml and 256 mg/ml for AB19606 and MRSA USA300, respectively. MOX alone and in combination with topical exosome-loaded gels resulted in significant (p ≤ 0.05) zones of inhibition compared to vehicles and untreated controls. Inhibition zone areas against MRSA USA300 and AB19606 ranged between 30-43 cm2.
Discussion: Our results demonstrated that MOX can be loaded into the topical exosome-loaded gels and has significant antimicrobial activity against two common wound pathogens. These results warrant future preclinical and clinical studies to substantiate their use in preventing or treating wound infections.
Acknowledgements: This work was supported by US Army Medical Research and Development Command Contract HT9425-24-P-0035. The views, opinions, and findings are those of the author(s) and should not be construed as official Army or DHA position, policy or decision unless designated by other documentation.

.jpg)