Practice Innovations
(PI-032) Innovate to Elevate: Reducing Pressure Injuries
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Glynnis Lowe, MSN, RN, NE-BC; Taylor Wolpert, BSN
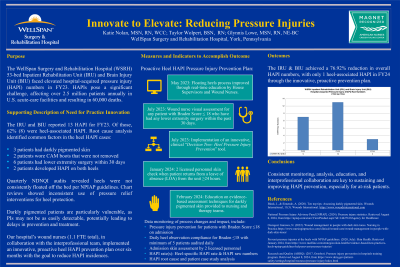
Introduction: Hospital-acquired pressure injuries (HAPIs) remain a critical challenge in healthcare, affecting over 2.5 million patients annually in the United States and contributing to 60,000 deaths. A 53-bed inpatient rehabilitation and brain injury unit experienced elevated HAPI rates in FY23, with 62% of reported cases being heel-associated. Root cause analysis revealed contributing factors such as darkly pigmented skin, inconsistent pressure relief interventions, and lower extremity surgeries. A proactive, targeted intervention was developed to address these risks and reduce HAPI rates.
Methods: A six-month proactive heel HAPI prevention plan was implemented. Interventions included:
Results: The unit achieved a 76.92% reduction in overall HAPI rates, with heel-associated HAPIs reduced to a single case in FY24. Daily heel observation compliance exceeded target benchmarks, and admission skin assessments by two licensed personnel improved consistency in early detection and intervention.
Discussion: This structured, proactive approach demonstrates the effectiveness of targeted interventions in reducing HAPI rates. The inclusion of education, interprofessional collaboration, and a clinical decision-making tool provided sustainable improvements in care. Special attention to vulnerable populations, such as patients with darkly pigmented skin, was critical in achieving these outcomes. This model can be replicated across similar settings to address HAPI challenges and improve patient safety and outcomes.
Methods: A six-month proactive heel HAPI prevention plan was implemented. Interventions included:
- Enhanced education on heel floating techniques and real-time process reinforcement.
- Targeted visual assessments for patients with Braden Scores ≤18 and recent lower extremity surgeries.
- Introduction of a clinical “Decision Tree: Heel Pressure Injury Prevention” tool.
- Implementation of two licensed personnel skin checks following patient leaves of absence ≥24 hours.
- Training on evidence-based assessment techniques for darkly pigmented skin. Outcome measures included compliance with heel observation protocols, adherence to skin assessments, and monitoring of heel-specific and overall HAPI rates. Data were collected and analyzed to assess the effectiveness of these interventions.
Results: The unit achieved a 76.92% reduction in overall HAPI rates, with heel-associated HAPIs reduced to a single case in FY24. Daily heel observation compliance exceeded target benchmarks, and admission skin assessments by two licensed personnel improved consistency in early detection and intervention.
Discussion: This structured, proactive approach demonstrates the effectiveness of targeted interventions in reducing HAPI rates. The inclusion of education, interprofessional collaboration, and a clinical decision-making tool provided sustainable improvements in care. Special attention to vulnerable populations, such as patients with darkly pigmented skin, was critical in achieving these outcomes. This model can be replicated across similar settings to address HAPI challenges and improve patient safety and outcomes.

.jpg)