Clinical Research
(CR-032) Interim Results from a Non-comparative Clinical Investigation Evaluating Tolerability of a Pressure Injury Prevention Protocol Incorporating a Silicone Border Super-absorbent Polymer Dressing in Long-term Acute Care Setting
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Chrystalbelle Rogers, MSN, RN, CWCN, CENP – Director of Clinical Services, Hartmann USA; Syed Naqvi, B.S. – Department of Population and Quantitative Health Sciences – University of Massachusetts Medical School; Anthony Nunes, PhD – Assistant Professor, Department of Population and Quantitative Health Sciences, University of Massachusetts Medical School
Introduction: Among patients in Long Term Acute Care (LTAC) hospitals, prevention of sacral pressure injuries requires clinical diligence due to prolonged immobility and higher prevalence of urinary and bowel incontinence. Approaches to preventing sacral pressure injuries may include complementary interventions such as manual rotation, pressure reducing devices, topical agents, and, more recently, dressings. The purpose of this study was to describe tolerability and effectiveness of a sacrum-shaped, multi-layer, silicone super-absorbent polymer dressing.
Methods: We conducted a prospective, non-comparative clinical investigation with qualitative endpoints. Patients receiving the dressing were evaluated and designated as high risk of developing sacral pressure injuries according to the Braden Scale or any other tool routinely used in the site. Dressing replacement was performed at the discretion of the clinical staff but no less than once every 7 days. Surveys of patients were conducted at baseline, at each dressing change, and upon exit from the study.
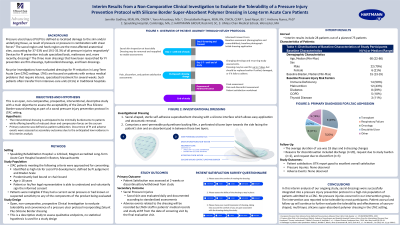
Results: From 1/2024 to 8/2024, 28 patients consented to participate in the dressing protocol. The median age of the participants was 60 (min 22, max 86) and the most common primary diagnoses included post-transplant (n=8), respiratory failure (n=7), and malignancies (n=6). The median Braden Score at baseline was 15 (interquartile range: 14-17). The average duration of use was 18 days consisting of 6 dressing changes. No pressure injuries were observed. Reasons for discontinuation included discharge (n=20), request due to study burden (n=2), and request due to discomfort (n=3). One patient discontinued due to an emerging serous-filled blister. Among patients completing an exit assessment, 87% reported that their overall experience with the dressing was good to excellent.
Discussion: In this interim analysis of our ongoing study, sacral dressings were successfully integrated into a pressure injury prevention protocol in a high-risk population of patients admitted to a LTAC. No precure injuries occurred in our intervention group and the intervention was reported to be tolerable by most participants. Patient accrual and follow-up will continue to further evaluate the tolerability and effectiveness of sacrum-shaped, multi-layer, silicone super-absorbent polymer dressing in the LTAC setting.
Methods: We conducted a prospective, non-comparative clinical investigation with qualitative endpoints. Patients receiving the dressing were evaluated and designated as high risk of developing sacral pressure injuries according to the Braden Scale or any other tool routinely used in the site. Dressing replacement was performed at the discretion of the clinical staff but no less than once every 7 days. Surveys of patients were conducted at baseline, at each dressing change, and upon exit from the study.
Results: From 1/2024 to 8/2024, 28 patients consented to participate in the dressing protocol. The median age of the participants was 60 (min 22, max 86) and the most common primary diagnoses included post-transplant (n=8), respiratory failure (n=7), and malignancies (n=6). The median Braden Score at baseline was 15 (interquartile range: 14-17). The average duration of use was 18 days consisting of 6 dressing changes. No pressure injuries were observed. Reasons for discontinuation included discharge (n=20), request due to study burden (n=2), and request due to discomfort (n=3). One patient discontinued due to an emerging serous-filled blister. Among patients completing an exit assessment, 87% reported that their overall experience with the dressing was good to excellent.
Discussion: In this interim analysis of our ongoing study, sacral dressings were successfully integrated into a pressure injury prevention protocol in a high-risk population of patients admitted to a LTAC. No precure injuries occurred in our intervention group and the intervention was reported to be tolerable by most participants. Patient accrual and follow-up will continue to further evaluate the tolerability and effectiveness of sacrum-shaped, multi-layer, silicone super-absorbent polymer dressing in the LTAC setting.

.jpg)