Case Series/Study
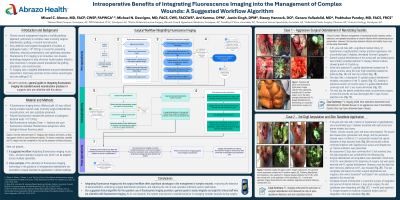
(CS-004) Intraoperative Benefits of Integrating Fluorescence Imaging into the Management of Complex Wounds: A Suggested Workflow Algorithm
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Michael Desvigne, MD FACS – Plastic Surgery; Arti Kamur, DPM – Podiatry; Heather Cole, MD – Trauma, Orthopedic Surgery; Justin Singh, DPM – Podiatry; Baljeet Uppal, MD – Vascular Surgery; Prabhakar Pandey, MD – Urology
Introduction: Bacterial Fluorescence Imaging* is an innovative, non-invasive technology designed to enhance the assessment of wounds by detecting bacterial contamination in real-time. This imaging system uses fluorescence to identify bacterial presence, helping clinicians locate bacteria linked to poor outcomes in complex wound procedures like amputation and reconstruction. It aids in targeted debridement and post-debridement assessment, improving outcomes across various wound types and care settings1,2,3.
Methods: A 10-patient case series presents examples of the utilization of this technology in the guidance of intraoperative debridement across multiple specialties. Wound types and pathologies include non-healing, dehiscent post-amputation wounds, surgical site infections, diabetic foot and pressure ulcers and necrotizing fasciitis. An algorithm for a suggested workflow that can be adapted to different surgical cases is provided.
Results: In surgical debridement, the fluorescence Imaging device* enabled real-time detection of bacterial presence, increasing its efficacy. In amputation, it helped identify bacterial presence in the residual limb, optimizing amputation level and wound management. During reconstruction, it optimized bacterial hotspot removal on graft sites prior to application. For all cases post-debridement verification of sufficient bacterial removal is encouraged. In the case of skin substitutes and grafts, documentation is particularly relevant in recording that optimal wound bed preparation was achieved for the graft to thrive.
Discussion: Integrating Bacterial Fluorescence Imaging into the intraoperative workflow offers significant advantages in the management of complex wounds. The technology improves the detection of bacteria (including in biofilm form), enhancing surgical debridement precision, and reducing the risk of postoperative infections and/or graft failure. Its real-time, its non-invasive capabilities make it safe and efficient, and its documentation capabilities help document the need for and optimal use of skin substitutes. As its use expands, this system may become a standard practice in managing complex wounds during surgery. This case series is meant to describe its benefit but also its ease of integration into a surgical workflow.
Methods: A 10-patient case series presents examples of the utilization of this technology in the guidance of intraoperative debridement across multiple specialties. Wound types and pathologies include non-healing, dehiscent post-amputation wounds, surgical site infections, diabetic foot and pressure ulcers and necrotizing fasciitis. An algorithm for a suggested workflow that can be adapted to different surgical cases is provided.
Results: In surgical debridement, the fluorescence Imaging device* enabled real-time detection of bacterial presence, increasing its efficacy. In amputation, it helped identify bacterial presence in the residual limb, optimizing amputation level and wound management. During reconstruction, it optimized bacterial hotspot removal on graft sites prior to application. For all cases post-debridement verification of sufficient bacterial removal is encouraged. In the case of skin substitutes and grafts, documentation is particularly relevant in recording that optimal wound bed preparation was achieved for the graft to thrive.
Discussion: Integrating Bacterial Fluorescence Imaging into the intraoperative workflow offers significant advantages in the management of complex wounds. The technology improves the detection of bacteria (including in biofilm form), enhancing surgical debridement precision, and reducing the risk of postoperative infections and/or graft failure. Its real-time, its non-invasive capabilities make it safe and efficient, and its documentation capabilities help document the need for and optimal use of skin substitutes. As its use expands, this system may become a standard practice in managing complex wounds during surgery. This case series is meant to describe its benefit but also its ease of integration into a surgical workflow.

.jpg)