Evidence-Based Practice
(EBP-003) Is Less Attention Being Paid to Treatment of Pressure Injuries at the Root of Hard to Reduce Hospital Acquired Bacteria or Sepsis?
Introduction: Hospital Acquired Infections are closely monitored reportable events. It could be possible that traditional HAI Surveillance is not by itself sufficient for determining the risks, mortality, and costs associated with treating critically ill patients. The relationship between HAI’s and underlying reasons and relationships to treatment require more analysis. Amongst HAIs, Blood Stream Infections (BSI), also classified for tracking purposes as sepsis and Hospital Acquired Bacteremia (HOB) are associated with notable degrees of mortality.
Methods:
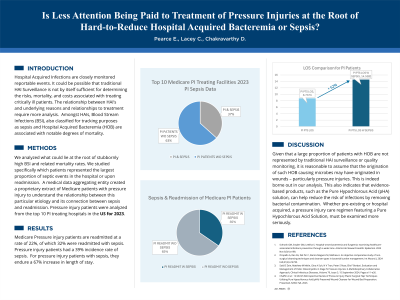
We analyzed what could lie at the root of stubbornly high BSI and related mortality rates. We studied specifically which patients represented the largest proportion of septic events in the hospital or upon readmission. A medical data aggregating entity created a proprietary extract of Medicare patients with pressure injury to understand the relationship between this particular etiology and its connection between sepsis and readmission. Pressure injury patients were analyzed from the top 10 PI treating hospitals in the US for 2023.
Results:
Pressure injury patients represent 79% of the readmitted patients of which, 33% were readmitted with sepsis. Pressure injury patients had a 40% incidence rate of sepsis. 85% of admitted/readmitted septic patients (includes both community + hospital acquired) had a pressure injury.
Discussion:
Given that a large proportion of patients with HOB are not represented by traditional HAI surveillance or quality monitoring, it is reasonable to assume that the origination of such HOB causing microbes may have originated in wounds - particularly pressure injuries. This is indeed borne out in our analysis. This also indicates that evidence based products, such as the Pure Hypochlorous Acid (pHA) solution that is a known and evidence based treatment to reduce the severity of/infection in pressure Injuries, whether pre-existing or hospital acquired, must be examined more seriously.

.jpg)