Case Series/Study
(CS-003) Lymphangioma Circumscriptum (LC): A Case Series Involving Gynecology-oncology, Plastic Surgery, and Complex Wound Management
Friday, May 2, 2025
7:45 PM - 8:45 PM East Coast USA Time
Julia McGee, BS – Tulane University School of Medicine; Jessica Reid, MS – Tulane University School of Medicine; Molly Gaffney, BS – Tulane University School of Medicine; Cameron Belding, MD – Tulane University School of Medicine; Katarina Stephanos, MS – Tulane University School of Medicine; Abigail Chaffin, MD, FACS, CWSP, MAPWCA – Tulane University School of Medicine
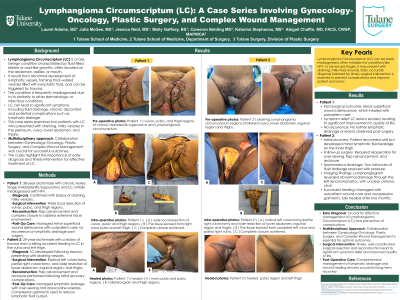
Introduction: Lymphangioma Circumscriptum (LC) is a rare, benign condition characterized by fluid-filled blisters or wart-like growths, commonly found on the abdomen, axillae, or mouth. It results from abnormal lymphatic vessels forming thick-walled vesicles filled with lymphatic fluid and can develop after trauma. This case series examines two patients with LC, presenting with draining, milky vesicles in the perineum, vulva, lower abdomen, and thighs. Through collaboration between Gynecology-Oncology and Plastic Surgery, both underwent complex surgical interventions focused on resection, reconstruction, and post-operative wound care. These cases emphasize the need for early diagnosis and a multidisciplinary approach.
Methods: The first patient, a 38-year-old female with chronic Hurley Stage 3 Hidradenitis Suppurativa and LC, was initially misdiagnosed with HPV. A biopsy confirmed LC, leading to a wide local resection of the vulvar, pubic, and thigh regions with flap advancement and complex closure. The second patient, a 29-year-old female with a history of trauma to the vulva and left thigh from a biking accident, developed LC. She underwent extensive surgery, including radical left vulvectomy, partial right vulvectomy, and wide resection of the lower abdomen, inguinal region, and thighs.
Results: The first patient experienced minor superficial wound dehiscence, which healed with outpatient care. The LC lesions were excised, leading to symptomatic relief and improved quality of life. No recurrence or lymphatic drainage was reported. The second patient initially recovered well but developed minor lymphatic fluid leakage on the inner thigh. She returned to the OR for over-sewing, flap advancement, and reclosure. Retrograde doxycycline sclerosis and an abdominal binder reduced lymphatic output. After discharge, two instances of spontaneous fluid drainage resolved with pressure. A lymphangiogram revealed abnormal drainage through the left renal lymphatics, and the cisterna chyli could not be clearly identified. The surgery was successful, and the patient demonstrated significant improvement. She was managed at the outpatient wound clinic with conservative treatment and lymphatic compression garments for approximately two months until fully healed.
Discussion: This case series highlights the need for a multidisciplinary approach in managing LC, often misdiagnosed as conditions like HPV. Timely diagnosis is crucial for effective management. Collaboration between specialties ensures comprehensive care and improved outcomes.
Methods: The first patient, a 38-year-old female with chronic Hurley Stage 3 Hidradenitis Suppurativa and LC, was initially misdiagnosed with HPV. A biopsy confirmed LC, leading to a wide local resection of the vulvar, pubic, and thigh regions with flap advancement and complex closure. The second patient, a 29-year-old female with a history of trauma to the vulva and left thigh from a biking accident, developed LC. She underwent extensive surgery, including radical left vulvectomy, partial right vulvectomy, and wide resection of the lower abdomen, inguinal region, and thighs.
Results: The first patient experienced minor superficial wound dehiscence, which healed with outpatient care. The LC lesions were excised, leading to symptomatic relief and improved quality of life. No recurrence or lymphatic drainage was reported. The second patient initially recovered well but developed minor lymphatic fluid leakage on the inner thigh. She returned to the OR for over-sewing, flap advancement, and reclosure. Retrograde doxycycline sclerosis and an abdominal binder reduced lymphatic output. After discharge, two instances of spontaneous fluid drainage resolved with pressure. A lymphangiogram revealed abnormal drainage through the left renal lymphatics, and the cisterna chyli could not be clearly identified. The surgery was successful, and the patient demonstrated significant improvement. She was managed at the outpatient wound clinic with conservative treatment and lymphatic compression garments for approximately two months until fully healed.
Discussion: This case series highlights the need for a multidisciplinary approach in managing LC, often misdiagnosed as conditions like HPV. Timely diagnosis is crucial for effective management. Collaboration between specialties ensures comprehensive care and improved outcomes.

.jpg)